James Raftery, freelance political analyst and researcher, explores the realities of COVID-19 testing in the UK
Antigen testing is a crucial element of public health responses to COVID-19 around the world. Countries such as South Korea and Germany have effectively used testing to control the pandemic. Britain’s government has been less successful in its approach to testing, although the establishment of a test and trace program is a valuable beginning.
Why is testing so important?
On an individual level, antigen testing – tests which check see whether you are currently infected with COVID-19 – is helpful because it allows people to know if they are have the virus. This can give workers the confidence to return to work if they have been worried about having symptoms, yet tested negative, and help businesses organise their staff.
Particularly important, asymptomatic screening can help identify cases where people are infected yet do not show symptoms. They are still at risk of shedding the virus and infecting others, but may not be self-isolating because they do not have symptoms. Even if people do develop symptoms, there is a pre-symptomatic transmission period of three days when they can still infect others. Testing can help such people know they have the virus and that they need to self-isolate.

On a national and regional level, widespread testing helps to give policymakers an insight into how many people in the country have the virus, and where they are regionally distributed. This is valuable since it can help to calculate the virus’ transmission rate R, and help to identify local outbreaks and centres of infection. This in turn can better inform policy responses.
Perhaps testing’s most vital use is as part of a testing, tracing and isolating system. This is a method of controlling the spread of the virus whereby symptomatic people are tested and quarantined, while investigatory teams trace their contacts to identify people who may be at risk. These people are themselves then asked to isolate, and may also be tested. If they are positive, then their contacts may also be traced. The benefit of this method of virus suppression is that – if it works well – then it can effectively identify and quarantine the infected to such an extent that there is no need for a general lockdown of the entire population.
Testing is obviously not, on its own, sufficient to combat the spread of the virus. It is not the sole reason why nations such as South Korea have had such success controlling the virus. It should be used in conjunction with a range of other policy measures, such as social distancing rules and mask wearing. However, the examples below illustrate the value that testing can have as part of a wider effective strategy.
What have other countries got right?
South Korea have an effective COVID-19 testing system. They began testing symptomatic people and their contacts early. Analysis has shown that an ideal level of testing results in roughly 3% of tests coming back as positive. Countries with this level, such as Vietnam and Australia tended to be more successful in controlling the virus. This is not to say that if a country can test to the extent that 3% of results are positive, then it will be able to control the virus, but it can give a guide to a good target level.
Less than a week after South Korean authorities detected the country’s first case of COVID-19 on January 20th, meetings were already taking place between health officials and 20 pharmaceutical and medical companies to ramp up the production and approval of test kits. It took just two weeks for the government to approve and distribute kits which were capable of producing results in under six hours.
South Korea had learnt lessons from previous coronavirus infections during the 2003 SARS outbreak and the 2015 MERS outbreak. South Korea suffered the highest number of cases from the latter save for Saudi Arabia. This was in part due to the government’s slow response and lack of testing capacity. The authorities learnt their lesson, and passed a law allowing for testing systems to be immediately approved if there was a crisis. Not only did South Korea have the capacity to ramp up testing rapidly, it crucially had the political will that allowed it to do so.
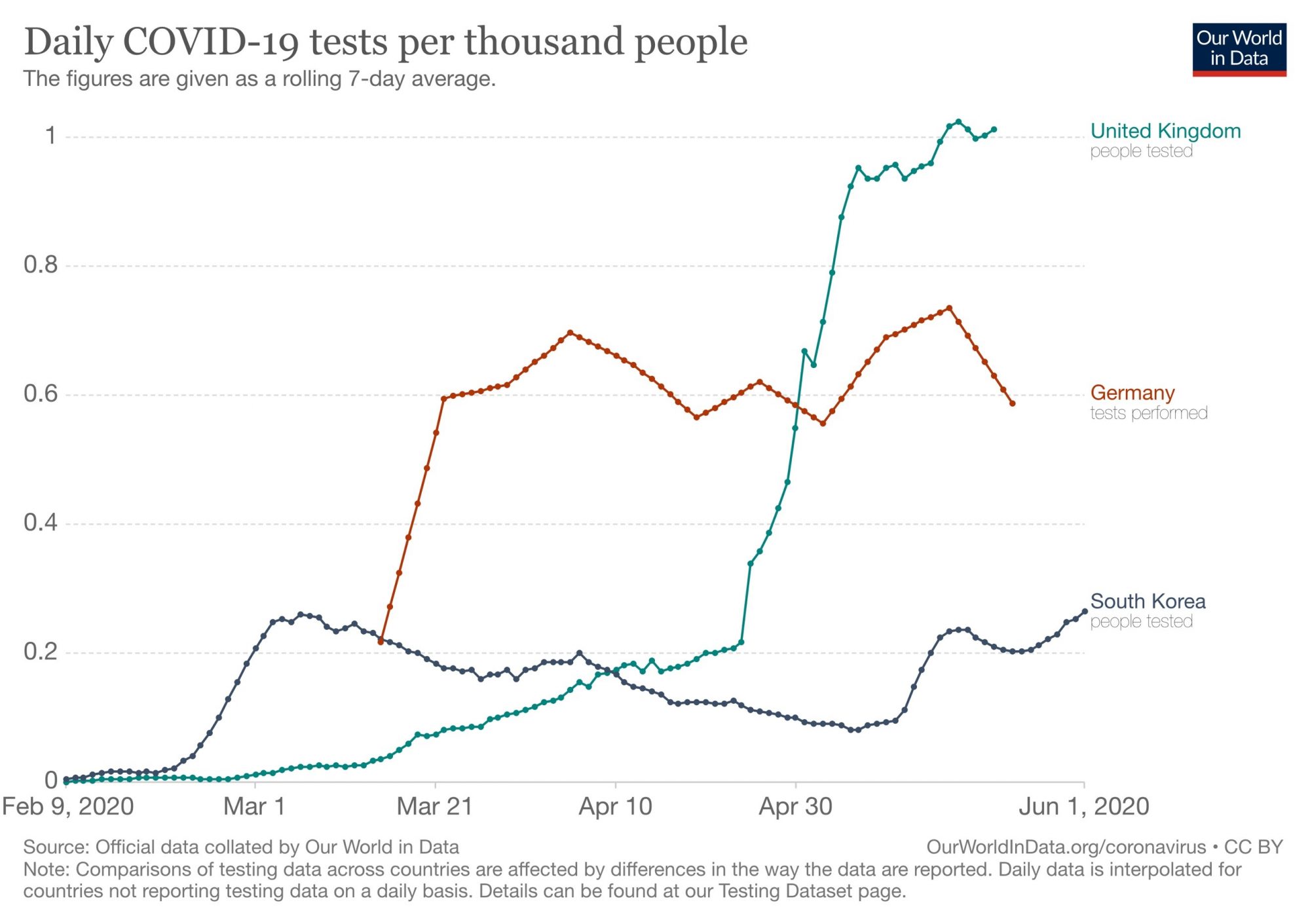
The graph below illustrates the benefit of such preparedness. South Korea could rapidly scale up its own testing capacity merely weeks after the first detections, until by mid-March it could test almost 20,000 people each day. This was crucial in halting the virus’ spread. From a peak of 909 new cases at the end of February, South Korea’s policy had remarkable success. By late March, there were only around 100 new cases each day. The last time the daily figure for new cases had three digits is now nearly 2 months ago, at the beginning of April.
 The success of the South Korean testing and tracking model inspired Germany’s own testing policy. Its goal is also to slow the spread of the virus by testing everybody who suspects they have contracted it. Before Germany had even had a positive test, a hospital in Berlin had developed a test and shared the formula online. This test was produced rapidly and then adopted by the WHO. By the time Germany had its first confirmed case in February, its laboratories had been able to stockpile a large number of kits.
The success of the South Korean testing and tracking model inspired Germany’s own testing policy. Its goal is also to slow the spread of the virus by testing everybody who suspects they have contracted it. Before Germany had even had a positive test, a hospital in Berlin had developed a test and shared the formula online. This test was produced rapidly and then adopted by the WHO. By the time Germany had its first confirmed case in February, its laboratories had been able to stockpile a large number of kits.
By April 6th, up to 300 German laboratories had been involved in their rapid testing program. Much like South Korea, the government also had efficient systems set-up and ready to go in preparation for a pandemic. When the Robert Koch Institute, Germany’s disease control and prevention agency, gave the go ahead, a pre-planned epidemic strategy kicked in. This detailed payment structures for labs to run diagnostic tests, which made it easier for the government to increase testing capacity at pace.
Also working to its favour was the German system’s decentralised structure. The RKI is not the only authority for testing. Instead, the 16 federal states make their own decisions, and thus have a more accurate picture of the extent of infection in each region. This also means that there are fewer coordination meetings and centralised hierarchies. Testing is done by local institutions, who are better connected and closer to the areas within which they are testing. In the words of the German government’s strategy, this has allowed its public health response to move from tests ‘that confirm the situation’ to tests that ‘get ahead of it.’
Germany is also one of a number of nations where scientists have been using a method called pool testing to increase labs’ testing capacity. This is where samples from a number of different people are pooled into one batch. This is then tested as a single sample would be. If this test is negative, then all the samples that went into that batch are confirmed as positive. If the test comes out positive, then the samples can be individually re-tested to determine which are positive and which negative.
This has the potential to dramatically increase the number of tests that can be done with a single kit. Researchers from the Institute for Medical Virology at the University Hospital Frankfurt and the German Red Cross Blood Donor Service estimated that this could increase testing capacity tenfold.

What has the UK done?
The UK’s record on antigen testing somewhat patchier. Relatively early on in the pandemic, the UK had a policy of testing and tracing the contacts of cases. This proved effective in the early days, when numbers where limited. However, it was abandoned on March 12, when the Prime Minister announced that community testing would cease, in favour of testing symptomatic cases in hospitals. Partly as a response to this announcement, the WHO implored countries to ‘test, test, test’ several days later.
SAGE papers reveal that the UK’s system of testing and tracing was stopped because even a handful of cases were causing too many problems for Public Health England’s systems. Advisors said on February 18 that PHE could only cope with testing and tracing the contacts of five cases per week, while estimating that this might only be able to scale up to 50 cases.
In part, this decision was a result of the government’s favoured approach of establishing large central hubs for testing, rather than utilising the UK’s large number of university, and private research and commercial labs. This approach made it more difficult to quickly scale up and carry out localised, community testing.
To make things worse, the government had a policy whereby hospital patients who did test positive could be discharged into care homes.
It also meant that many care home residents and workers, even if they were symptomatic, could not access testing. To make things worse, the government had a policy whereby hospital patients who did test positive could be discharged into care homes. This exacerbated the growing epidemic in care homes, at a time when care homes found it very difficult to access testing.
Realising the importance of testing, the government set itself a number of testing targets in an effort to increase the UK’s testing capacity. For example, Health Secretary Matt Hancock set a target of testing 100,000 people daily by the end of April. Although this motivated a dramatic increase in testing capacity in that month, the target was not met, with only 73,191 people receiving an antigen test for COVID-19 on April 30. The graph above clearly shows how testing levels increased rapidly in the UK throughout April.
On May 11, the government published its strategy for dealing with COVID-19. This acknowledged the importance of a testing and tracing policy. On May 31, the government claimed it had made its target of 200,000-test capacity a day early. However, it has been criticised for the statistical reporting of testing numbers. Double-counting of nose and saliva swabs from one person, and including tests that have been posted out to labs or homes but not yet returned, both diminish the validity of daily reported figures for the number of tests. For days now, the government has been unable to publish the number of people tested per day. This lack of clarity has made it more difficult to effectively establish the government’s track and trace program, and hindered the efficacy of its response.
How could the UK improve?
The government’s efforts in using testing and tracing to contain the spread of the virus have been described as ‘too little, too late, too flawed’ by the British Medical Journal. However, there are a number of ways in which the UK’s approach could improve.
Firstly, clear and regular statistics on the number of people tested daily, rather than on number of tests taken or sent out, would help to give more confidence to test and trace system. Secondly, this system needs to be professionally set up and operated. There have been a number of problems with the system, such as a faulty app and contact tracers not being made aware that their shifts were starting. Thirdly, as the BMJ suggested, the system should be resourced and staffed properly and decentralised. This will make sure that contact tracing teams are led by professionals who know their communities and local extents of the outbreak.
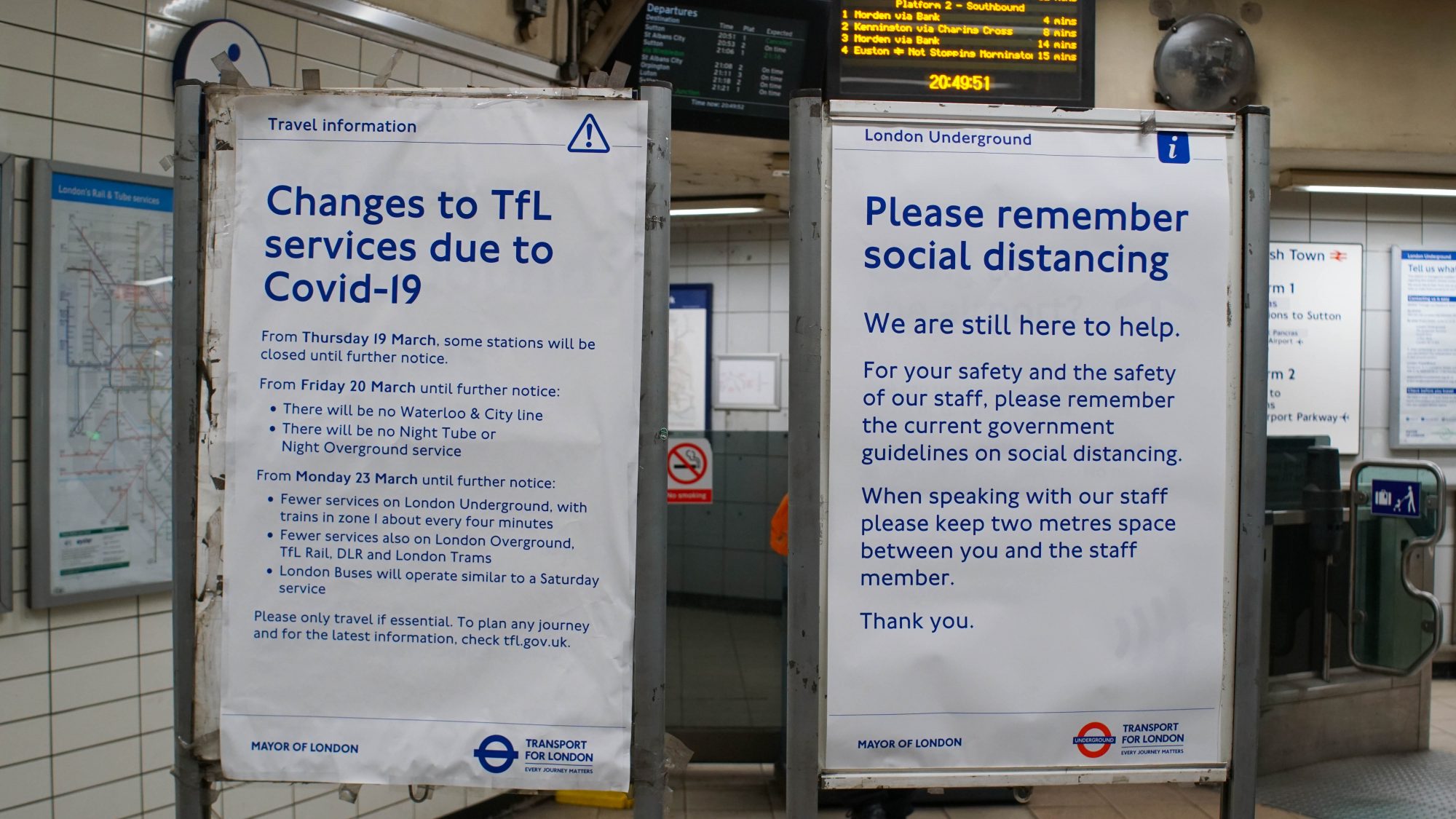
Finally, the government must ensure that its message around testing and tracking is clear. The system only works if people comply, isolating if they are instructed to do so. There have been fears recently that the government’s communication around isolation and lockdown has been unclear and unfocussed. It needs to speak clearly and with one voice to effectively convey the importance of isolation as part of its strategy against COVID-19.