Prof Dr Freimut Schliess, Director of Science & Innovation at Profil Institut für Stoffwechselforschung GmbH explains the important role of innovation when it comes to healthy living and active ageing, including his thoughts on the diabetes paradigm
The International Diabetes Federation estimates that 66 million people have diabetes in Europe – with a rising trend towards 81 million people by 2048. Diabetes is a hub for co-morbid conditions and triggers frailty, pre-mature ageing and death from any cause. Today a woman who becomes diagnosed with diabetes at the age of 50 will lose almost seven years of her life, owing to diabetes.
Societal investments in healthy living and active ageing are key when aiming at reducing the relative risk of premature mortality from major chronic diseases by 25% before 2025 (as declared by the WHO) and increasing healthy lifespans by two years by 2020 (as envisioned by the European Innovation Partnership on Active and Healthy Ageing). The European Institute for Innovation and Technology (EIT) has recently implemented the EIT Health Knowledge and Innovation Community – a public-private partnership specifically dedicated to accelerating entrepreneurship and innovation for healthy living and active ageing in Europe.
Diabetes provides lots of room for rewarding innovations in healthy living and active ageing: the most important disease trigger is highly modifiable, pathogenetic transitions are potentially reversible and self-management plays an outstanding role in diabetes management. Therefore, one obvious strategy to prioritise investments in healthy living and active ageing would be to focus on the prevention and management of diabetes. This would have a profound effect on the overall chronic disease burden and be particularly effective in promoting healthy living and active ageing in Europe.
A life and disease course approach to diabetes
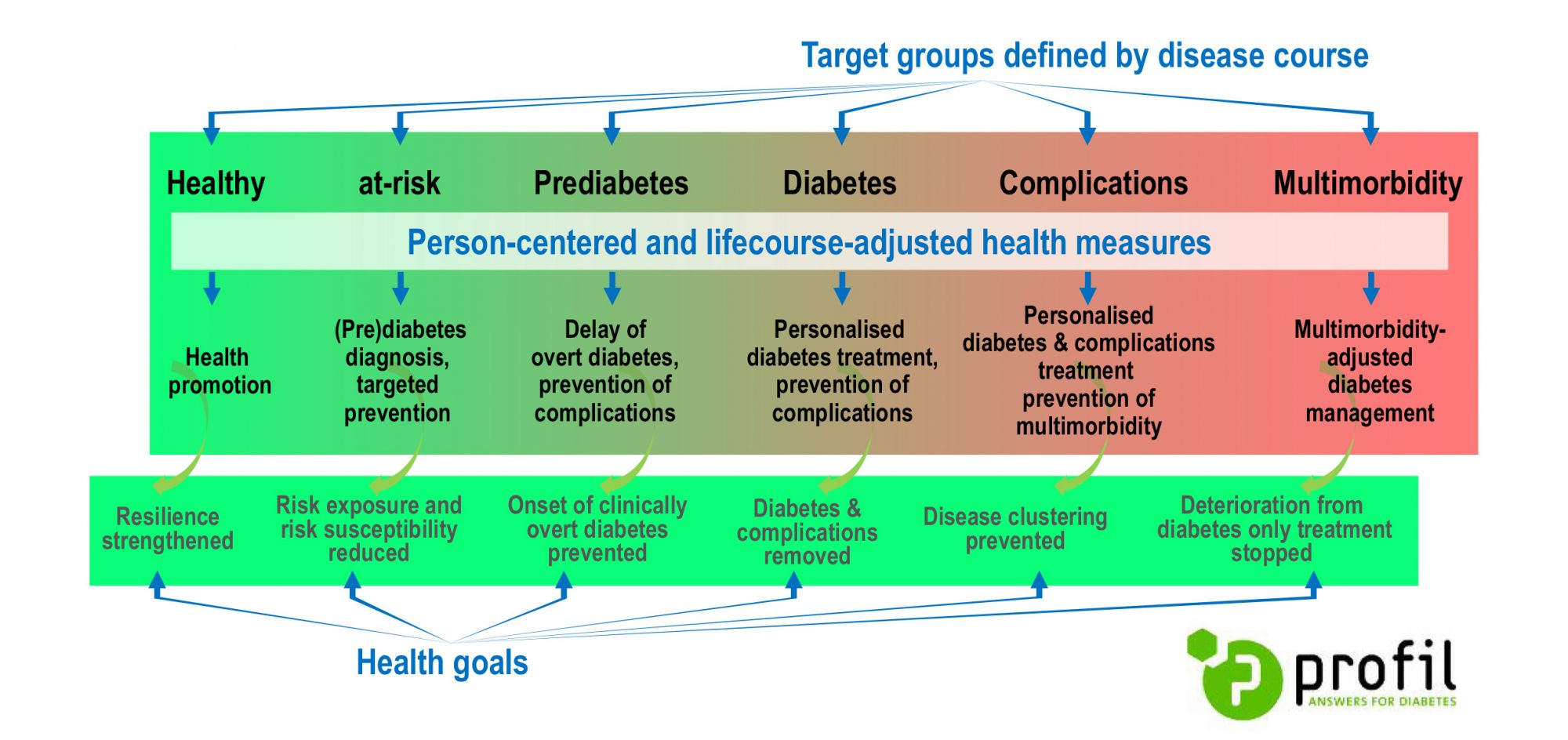
Following a combined life- and disease course approach may help to fully exploit the potential of innovations in diabetes (see the Figure): innovations in health promotion, diabetes prevention and diabetes management should be adjusted to the peoples socio-cultural and socio-economic background, as well as to biological signatures, the functional status and self-perception of health-related quality of life. In older age, adding quality of life to the amount of life and function to chronic disease may become an increasing priority. We suggest a strong commitment with the EMA geriatric medicines strategy, highlighting the specific needs of elderly people.
People-centred health promotion
Challenges. European living and working environments are obesogenic. They inherently pose disease risks by promoting physical immobility and unhealthy food choices. Education on how to prevent frailty and disability at an older age is underdeveloped. There is a gap between available knowledge and public awareness of disease-promoting behaviour.
Space for innovations. Policies for implementing anti-obesogenic living environments are needed. Housing design should support a long-lasting preservation of personal autonomy and societal participation. Health promotion at work has the potential to reach a large part of the population, but strategies for improving the sustainability of worksite health promotion measures are needed. A clear labelling of processed food products should indicate the health risk imposed by them. Healthy food choices should be facilitated by responsible food advertising and presentation. Products and services integrating social media, tele-coaching and the Internet of Things (IoT) and services could be tailored for specific target groups and allow for a benchmarking with peer groups. There are challenges to be overcome in regard to scalability, interoperability and privacy protection.
Person-centred diabetes prevention
Challenges. Glucocentrism does not meet the entire complexity of diabetes and inherently limits the efficacy of current diabetes prevention. Available tools do not effectively differentiate between metabolically healthy obese and obese people at risk. They identify neither lean, but metabolically obese people, nor people with sarcopenic obesity. Also, tools specifically addressing the frailty and morbidity risk of the elderly are not yet established. Lifestyle interventions appear to be inefficient outside of clinical trials.
Space for innovations. The overarching goal of new tools and services for preventing diabetes should be to stop the progressive loss of beta cell function. Interception with pro-diabetic transitions much before glycaemic criteria of pre-diabetes are met, will be key to increasing the effectiveness of diabetes prevention. A pre-diabetes taxonomy, based on genetic and metabolic signatures, will improve our understanding of the diversity in (pre)diabetes traits. We need tools that replace a rigid allocation of people to chronological age groups by a classification referring to states of biological and functional ageing.
Also, a thorough consideration of individual life characteristics, goals and preferences will optimise the precision fit of diabetes prevention measures. Digital solutions providing specific feedback loops, based on the processing of individual health and behavioural data will help to reach and motivate relevant target groups, and to incentivise the achievement of individual health goals.
Patient-centred diabetes treatment and prevention of co-morbid conditions
Challenges. A curative therapy of diabetes preventing co-morbid conditions is still missing. Closing the loop between blood glucose assessments and insulin dosing still depends on patients’ action. Particularly in the elderly, this accounts for extended periods of dysglycaemia that pose a considerable risk of frailty and physical (falls and fractures) and mental (cognitive impairment, dementia) disability. Many people with diabetes fail to reach their treatment goals – despite the plethora of therapeutic approaches that are available today.
Space for innovations. Sensor-based technologies for the collection of digital biomarkers and predictive algorithms may facilitate an early identification of patients with a high risk of co-morbid conditions. Drugs that protect beta cells from death and/or stimulate endogenous beta cell regeneration will greatly improve life quality and clinical outcome in people with diabetes. Future insulin sensitisers should refer to a full understanding of insulin resistance – particularly in the process of ageing. Artificial Pancreas systems will approach a “technical cure” of diabetes by mimicking the closed-loop metabolic control of blood glucose levels seen in healthy people. There is a trend towards integrating the prescription of drugs and devices within value-based schemes of chronic care provision, such as an integrated personalised diabetes management coupled to pay for performance compensation models.
Co-morbidity-adjusted diabetes management
Challenges. The top 10% of patients with Type 2 diabetes that incur the highest costs are likely to bear a high co-morbidity burden, to be on insulin therapy and to suffer from obesity and hypertension. Here, treatment guidelines focused on diabetes may conflict with co-morbid conditions, resulting in adverse interactions between drugs and diseases, non-compatible management strategies, polypharmacy and cost inefficiencies. In real-life conditions, treatment-effect-modifiers contribute to the well-known discrepancy between drug efficacy in clinical trials and drug effectiveness observed in everyday clinical practice.
Space for innovations. Improving the strength of primary care may immediately translate into lower rates of avoidable hospital admissions and fewer years of life owned to diabetes. Integrated personalised diabetes management programmes should pursue a proactive release of high-quality chronic care, focused on the outcome.
The telemedical consulting centre will have a high potential to ensure high-quality care especially in areas of rural depopulation with a high proportion of old people, and a low density of diabetic care practices. Predictive models will become available that balance individual life expectancy against lag time to benefit from specific interventions, based on signatures of biological ageing, as well as the patient-specific shaping of functional impairment and co-morbid conditions. Tools are required predicting the interaction of drugs at the levels of pharmacokinetics, pharmacodynamics, as well as safety and tolerability.
Perspective
Although diabetes is a paradigm case for rewarding innovation in healthcare, open and collaborative knowledge and innovation communities such as EIT Health are needed to fully translate societal investments into a tangible impact for European citizens. The coordinated curation of innovation portfolios targeting healthy living and active ageing, as well as the elimination of general obstacles to innovation, can be achieved best in close interaction with societal stakeholders. An inherent integration of close-to-market research, education & training and the creation of new businesses (EIT knowledge triangle) will greatly support innovators in diabetes to make a triple impact – on the healthcare experience of individual patients, the health of populations, and the sustainability of healthcare systems.
Please note: this is a commercial profile
Prof Dr Freimut Schliess
Director, Science & Innovation
Profil Institut für Stoffwechselforschung GmbH
Tel +49 2131 5018 225











