James Cotterell, Director at BBI Healthcare, argues that prescribing products that treat low blood sugar with a precise and measured dose of glucose can improve patient outcomes, reduce patient anxiety and save the NHS money
For people with diabetes who have previously relied on sugary food and drinks to treat low blood sugar, the sugar tax introduced in the UK on April 2018, has resulted in confusion and concern.
Managing and preventing low blood sugar is part of daily life for people with diabetes. Most people with Type 1 diabetes have episodes of low blood sugar (when their blood glucose level drops below 4mmol/L) often, around twice a week.1
One of the first things people learn after they have been diagnosed is why hypos happen and what to do about them. Common symptoms are: feeling shaky, sweating, hunger, tiredness, blurred vision, pins and needles around their mouth, finding it hard to concentrate, headaches, feeling tearful, increased heart rate, and becoming stroppy or stubborn. When this happens many people with diabetes eat or drink something sugary – for example, a sugary drink, such as fruit juice or an ordinary (non-diet) fizzy drink.
The sugar tax has implications for people with diabetes
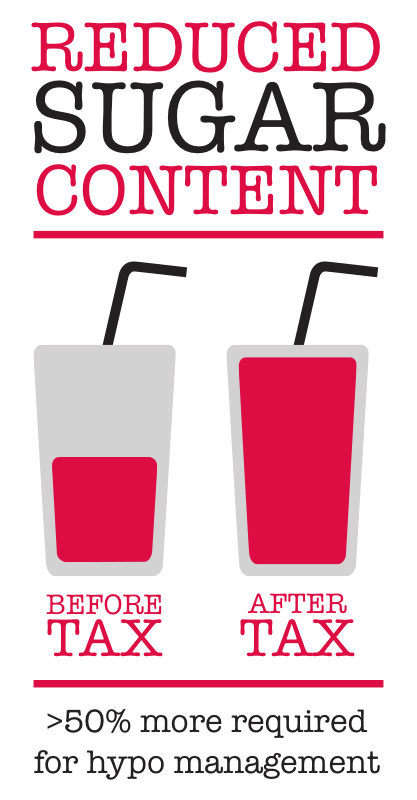
The sugar tax applied to soft sugary drinks, introduced in April 2018, has caused concern amongst people with diabetes. Previously able to rely on the amount of glucose in a bottle of drink, such as Lucozade, the sugar content in sugary drinks has been reduced by 50%. In real terms, this means that people with diabetes have to consume more of these drinks to receive the same amount of glucose.
Diabetes UK supports sugar reduction, but the charity is aware that these measures have caused concern for people who may use sugary food and drinks to treat low blood sugar. Diabetes UK states: “It won’t always be clear if and when companies have reduced the sugar content of their food and drinks, and they may not publicise any changes. When a company changes the sugar content, there may be a time when both old and new recipes of the same product are on sale at the same time, as the old recipe sells out.2
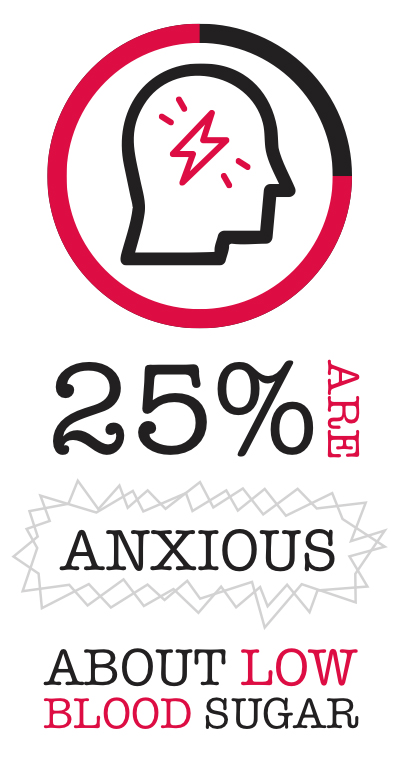
Anxiety about low blood sugar is a serious problem for 25% of people with diabetes3
Of course, it would be unwise to have no fear of hypoglycaemia at all – it’s a dangerous situation, and fear obviously plays some role in avoiding it. The effects of low blood sugar can be frightening, embarrassing, uncomfortable, unpleasant, or in their worst cases, fatal. But anxiety and fear about low blood sugar can result in people with diabetes deliberately running blood sugar levels higher than usual, which can result in elevated HbA1c and further complications and costs for the NHS.4, 5 In fact, the majority of diabetes-related conditions such as heart disease, nerve damage and amputation, and vision problems – occur as a result of uncontrolled blood glucose levels, particularly elevated blood sugar over a prolonged period of time.6
Low blood sugar has a significant negative impact on patient outcomes, healthcare resource use, and expenditure7
Whilst most hypos are mild, some can be severe. If improperly treated, low blood sugar can cause seizures and result in people collapsing or passing out.
In 2015, the mean cost per hospital admission for severe hypos in England was shown to be £1,034, and it is estimated that severe hypos currently cost the NHS £13 million a year.7 Effectively managing and treating low blood sugar with a measured and specific amount of glucose could prevent more serious complications and reduce the burden on secondary care.
Ensure people with diabetes have the right amount of glucose when they need it most
Having access to the right amount of glucose to confidently self-treat and self-manage low blood sugar levels are crucial for anyone living with Type 1 diabetes.
15-20g of fast-acting glucose is recommended to treat a hypo.8 GlucoGel contains a precise, measured, fast-acting glucose to help rapidly raise blood sugar levels and is recommended by NICE9 and the Joint British Diabetes Societies (JBDS) for hypo management.10
The Gluco range also includes a juice (GlucoJuice contains precisely 15g of fast-acting glucose) and dextrose tablets (GlucoTabs contain 3.7g of fast-acting glucose per tab) which are readily available at pharmacies and provide a measured alternative to the more traditional energy drinks and bars that are used to manage blood sugar levels.
Conclusion
The sugar tax may lead people with diabetes to doubt the amount of glucose they are absorbing. With anxiety about low blood sugar being a serious issue for people with diabetes, prescribing GlucoGel – a precise and measured dose of glucose – could help alleviate some of this concern and potentially reduce complications and costs arising from people with diabetes deliberately running blood sugar levels higher than usual.
Low blood sugar can result in serious complications if improperly managed, leading to poorer patient outcomes and ultimately increasing the burden on the NHS. An estimated £14 billion is spent a year on treating diabetes and its complications11, with the cost of treating complications taking the largest slice of the pie. By prescribing a precise and measured dose of glucose for people with diabetes, and taking a more precise approach to hypo management, we could improve patient care and save the NHS money.
For more information about the benefits of prescribing GlucoGel go to Getglucogel.co.uk
Please note: this is a commercial profile
References:
1 NHS, The Hospital Management of Hypoglycaemia in Adults with Diabetes Mellitus, March 2010 available at http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_Hypo_Adults.pdf accessed 26.10.18.
2 Diabetes.co.uk, Sugar reduction and hypo treatments: Frequently Asked Questions available at https://www.diabetes.org.uk/professionals/position-statements-reports/type-2-diabetes-prevention-early-identification/prevention-of-type-2-diabetes-whole-society-interventions-to-reduce-obesity/soft-drinks-industry-levy-faqs accessed 01.10.18.
3 Diabetes.co.uk, Managing Hypo Anxiety available at https://www.diabetes.org.uk/guide-to-diabetes/life-with-diabetes/hypo-anxiety accessed 01.10.18.
4 Diabetes.co.uk, Fear of Hypoglycaemia available at https://www.diabetes.co.uk/fear-of-hypoglycemia.html accessed 01.10.18.
5 Leiter L, et al., Can J Diabetes. 2005;29(3):00-00.
6 Philip McEwan, Healthcare resource implications of hypoglycemia-related hospital admissions and inpatient hypoglycemia: retrospective record-linked cohort studies in England, 2015
7 Diabetes.co.uk, Diabetes Complications available at https://www.diabetes.co.uk/diabetes-complications/diabetes-complications.html accessed 26.10.18.
8 Vindedzis et al. (2012).
9 NICE, Treatment of hypoglycaemia available at https://bnf.nice.org.uk/treatment-summary/hypoglycaemia.html accessed 01.10.18.
9 Joint British Diabetes Societies for Inpatient Care (JBDS-IP) The Hospital Management of Hypoglycaemia in Adults with Diabetes Mellitus. 3rd edition. April 2018.
10 Kanavos, van den Aardweg and Schurer: Diabetes expenditure, burden of disease and management in 5 EU countries, LSE, Jan 2012.
11 Diabetes.co.uk Cost of Diabetes, available at https://www.diabetes.co.uk/cost-of-diabetes.html accessed 09.11.18
James Cotterell
Director
BBI Healthcare
Tel: +44 (0)16 5686 8930