Gareth Jenkins, a partner at Changeology Group Ltd, discusses the potential of detailed analysis to enhance the efficiency of cancer care within the NHS
NHS cancer services face significant challenges, with growing patient backlogs and increasing demand putting immense pressure on resources. As trusts strive to manage capacity and reduce waiting times, additional funding alone will not solve these issues. Underlying operational inefficiencies, poor resource allocation, and underutilised capacity are key drivers that must be addressed to ensure sustainable improvements in patient care.
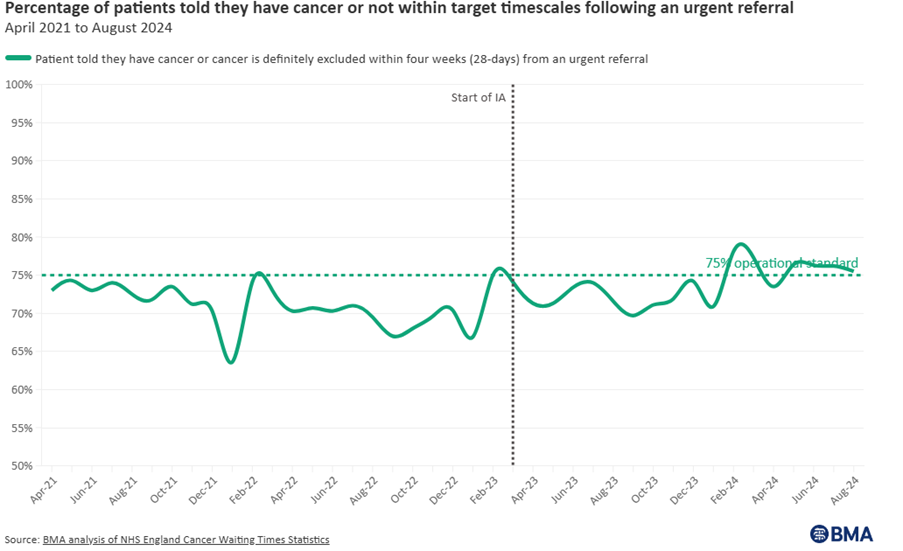
In a BMA article published on the 10th October 2024 NHS backlog data analysis, despite the changes in the cancer care targets, services continue to operate well below operational standards.
To tackle these challenges, NHS leaders increasingly turn to data-driven diagnostic tools such as Current State Analysis (CSA) and the Management Operating System (MOS). These tools offer actionable insights into how services currently operate, enabling trusts to implement targeted improvements that enhance efficiency, reduce costs, and improve patient outcomes.
The power of Current State Analysis
A CSA is the foundation of any successful operational transformation. It thoroughly examines existing processes, resource utilisation, and performance metrics, clearly showing how an organisation currently functions. In the context of NHS cancer services, CSA is particularly valuable for identifying inefficiencies that may not be immediately apparent but significantly impact service delivery.
Turning insights into action with the Management Operating System
Once a comprehensive CSA has been completed, the next step is to turn these insights into actionable improvements. This is where the MOS comes in. MOS provides a structured framework that aligns clinical priorities with operational efficiency, ensuring improvements are implemented and sustained over the long term.
Leveraging technology for smarter decision-making
Advanced analytics and simulation modelling are crucial tools in optimising NHS operations. These technologies allow trusts to predict outcomes, model scenarios, and refine resource allocation strategies before implementing changes.
- Predicting outcomes: Simulation models help test different operational scenarios – such as changes in scheduling or resource distribution – before rolling them out in real life.
- Data-driven decision-making: Real-time dashboards and reporting tools provide leaders with up-to-the- minute insights into performance metrics, ensuring informed decision-making.
By employing these technologies, trusts can proactively manage their resources and respond to challenges with agility.
In a recent HODU project undertaken by Changeology, simulating modelling was instrumental in delivering:
- Overtime hours reduced by 65%.
- Patient throughput increased by 20%.
- Wait times reduced by 30%.
- Staff satisfaction improved by 40%.
- Unit costs decreased by 8%.
Case Study 1: Transforming catheter labs to increase capacity
- Late starts: Over 41% of procedures began late, resulting in the loss of 1,000–1,500 hours annually. This translated into approximately 500 missed procedures each year.
- Underutilisation of sessions: The analysis showed that between 20% and 37% of operational capacity was being wasted, with up to 52% of available time left unused.
- Ineffective spending controls: While some sessions exceeded expectations, 44% underperformed, indicating poor planning and inconsistent resource allocation.
Addressing the root causes of late starts alone could potentially add 500 procedures per year without increasing resources. These insights enabled the Trust to streamline operations and significantly increase throughput, improving patient care and operational efficiency.
Case Study 2: Regional NHS cancer care transformation in endoscopy services
In collaboration with Lancashire and South Cumbria ICB and Cancer Alliance, Changeology led a comprehensive overhaul of endoscopy services across four NHS trusts. The results were significant:
- 21% regional activity increase.
- 27% reduction in waiting lists.
- £4.9 million in cost avoidance.
- 78% decline in patient breaches. These interventions increased patient throughput and fostered a sustainable, long-term model for operational excellence.
Long-term benefits of diagnostic-led transformation
While the immediate benefits of CSA and MOS include reduced waiting times and cost savings, the long-term impact is equally important:
- Improved patient outcomes: Optimised workflows lead to faster, more efficient care delivery, improving overall patient satisfaction and outcomes.
- Enhanced staff experience: Reducing operational inefficiencies decreases staff stress, improves job satisfaction, and helps retain talent.
- Sustainable change: Embedding continuous improvement into the Trust’s culture ensures that the benefits of CSA and MOS are sustained over time.
Conclusion: A sustainable path forward for NHS cancer care
Trusts cannot afford to delay operational changes if they are to meet the growing demand for NHS cancer care. By adopting data-driven diagnostic tools like CSA and implementing the MOS, trusts can unlock hidden capacity, reduce waiting times, and improve patient care – all without requiring additional resources.
The path forward lies in embracing sustainable, operational transformation. With the right tools and processes in place, NHS cancer services can recover from current pressures and thrive in the future, delivering the best possible care to every patient who requires it.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.