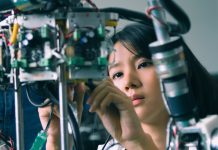
Rob Banathy, Senior Product Manager at NHS Digital, explains how his team developed a lateral flow device digital reader service that can detect nearly twice the number of positive COVID-19 cases during early infection compared to the human eye
At the start of 2021 when the government rolled out the use of self-conducted and reported lateral flow devices (LFDs) to support mass asymptomatic testing for the public, a concern was identified around users interpreted the test incorrectly, particularly when the lines on the LFDs are faint.
In this scenario, asymptomatic users might not be identified and may contribute to a chain of transmission. This is particularly a concern where testing is used in situations such as entry to nursing homes, where the impact of missing asymptomatic users could be devastating. To help mitigate this risk, we explored whether a digital reader could be used to interpret the result of an LFD more accurately by removing the variation in human eyesight and human bias.
Our approach
After searching for suppliers with the technology we needed, we discovered there were no production-ready, clinically assured solutions available in the market. We worked quickly with suppliers, and public health and regulatory teams, to design and test a service that could be used safely and effectively by the general population.
Following a proof of concept and technical evaluation stage, we chose a supplier and developed a pilot service that used artificial intelligence to interpret the test result from a photo submitted by the user. Consequently, the service is categorised as ‘software as a medical device’, which meant that we needed to conduct a clinical trial to prove the accuracy, safety, accessibility and effectiveness of the service.
The challenges
There were several challenges to overcome before we could deliver this service. Mindful of inclusivity and accessibility needs, we pursued a web service approach rather than a native app approach. Our goal was to provide a service that anyone with an internet-connected device with a camera could use, without the need to download any software or app. Due to the limited photo quality validation that this approach allowed, we relied heavily on user research to understand how we could design the service to meet user and public health needs to deliver a simple to use, accurate and scalable web service.
To overcome these challenges, collaboration and working openly across teams, organisations and delivery partners were key. We adapted our user research methods to work remotely and built prototypes to not only test our understanding of user and public health needs but also to demonstrate our emerging service vision with our policy and public health colleagues. We were supported by a range of teams, in areas such as regulatory, service design, information governance, security, commercial, policy, public health and science.
The pilot
During the pilot, we collected over 100,000 images from adult social care homes and NHS primary care staff as they reported their LFD results. We conducted extensive user research with these users, gaining valuable insight into user behaviours and expectations.
We worked with public health colleagues to verify our methods and our research data. We submitted our evidence to the Medicines and Healthcare products Regulatory Agency (MHRA) and sought their authorisation to use this ‘software as a medical device’ service.
We received authorisation in April 2021 and launched the LFD digital reader service in June 2021 to a small number of user cohorts. This helped us respond to the needs of users prior to scaling up a nationally available LFD reporting service.
The results
The LFD digital reader service has now been live for 12 months with more than 7 million digitally read results. Since launch, we’ve gained regulatory authorisation for all government-provided LFD types used for self-reporting.
We have conducted a service evaluation using real-world data from our production service. From the evaluation, it’s been demonstrated that the service outperforms self-read LFD reports by detecting nearly twice the number of true positive cases during early infection when the viral loads tend to be lower, and over 25% more true positives cases when viral loads are higher. This makes a significant impact in breaking the chains of transmissions and protecting those most vulnerable.
The service evaluation data also shows that the average time for a user to complete reporting their LFD result using the digital reader service is approximately the same as when a user manually reports their result.
What we’ve achieved
We’ve demonstrated how innovative technology can be used safely and effectively in a general population setting to increase the accuracy of interpreting LFD results and thereby improve public health outcomes. Continual access to user research and user behaviour data has guided our service design to ensure our service meets user needs.
Having clear goals was essential and it allowed us to work collaboratively with academics, clinicians, and technology and regulatory specialists to deliver an innovative idea from proof of concept to a full production service used by thousands of users every day.
The UK Health Security Agency has since recommended the availability of the service to all users reporting government-provided lateral flow tests.