Dr. Annabelle L. Fonseca et al explain the problems created by current medical guidelines for diagnosing pancreatic cysts
More than 2% of abdominal computed tomography (CT) scans will show a cyst in the pancreas. What to do about these cysts can sometimes leave us in a quandary.
Intraductal papillary mucinous neoplasms (IPMNs) are the most common type of pancreatic cyst that may harbour cancer or develop into cancer. This is a relatively new disease, first identified in 1982, and while our approach to these tumours has evolved since then, many patients still receive unnecessary treatment and we clearly still have a long way to go.
What are IPMNs?
IPMNs are cystic tumours that grow within the pancreatic duct and are characterised by the production of thick viscous mucous. The main pancreatic duct runs down the centre of the pancreas and gives off smaller branching ducts. IPMNs arise from either the main pancreatic duct or one of the branching ducts.
With the increasing use of CT scans, IPMNs are being diagnosed more frequently. Because we did not know enough about the natural history of the disease, and because of the terrible prognosis associated with pancreatic cancer, our tendency was to resect most IPMNs.
What do we know about IPMNs and the risk of cancer currently?
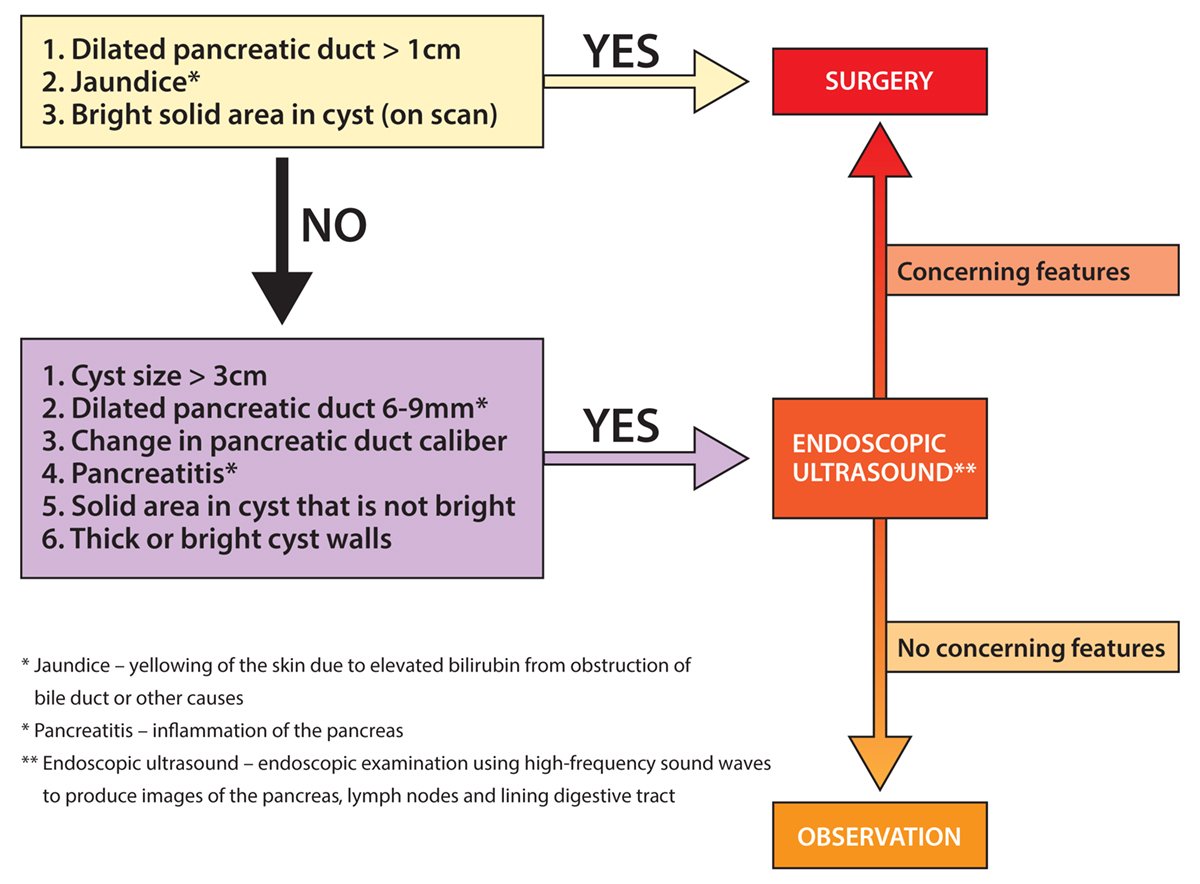
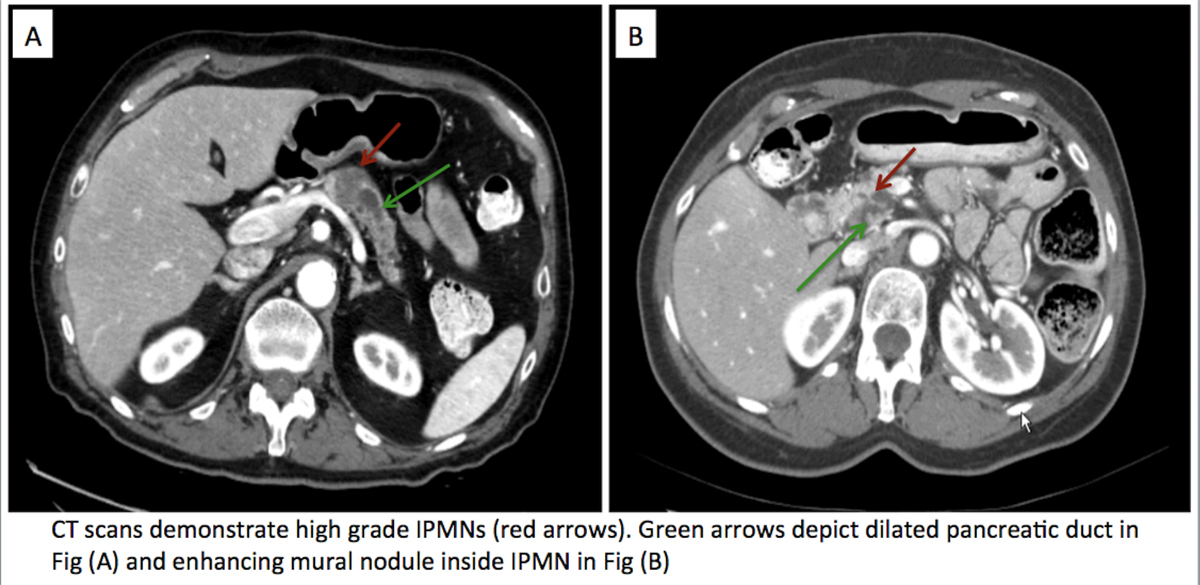
IPMNs with high grade dysplasia or a cancer component are ideally the ones to remove. Over the past decade we have learnt that specific findings on CT or other imaging can be used to help us with our decision (Figure 1). We currently follow recommendations based on expert consensus to help us decide which of these tumours we should take out. We know that IPMNs that develop from the main duct are at a higher risk of developing into cancer. We use imaging criteria and clinical findings to decide whether to operate, proceed with additional investigation, or to continue to monitor patients (Figure 2).
Current guidelines have created a dilemma
These guidelines help us to decide which patients would benefit from an operation. However, they also lead to us operating on many patients with IPMNs that would likely have never turned into cancer. The ability of current guidelines to accurately diagnose the presence or absence of high grade dysplasia or cancer ranges from 50-80% according to studies. This means that when we use these guidelines, the proportion of patients that we “over treat” is not insignificant, and we will also miss some patients that do have IPMNs with high grade dysplasia or cancer. This is a problem that we, and several other researchers around the world, are studying.
Current areas of research:
We know that IPMNs are associated with specific genetic mutations. However, these do not necessarily differentiate between those with different risks of becoming cancer. Additionally, this information is usually obtained from the tissue after resection, and this does not help us to decide who needs an operation. Cyst fluid analysis is an exciting area of research, where fluid is obtained during an endoscopic ultrasound, and can then be tested for different biological markers that may help in our pre-operative decision making. Radiographic imaging is also being studied at a more granular level in the field of radiomics, which is the high throughput analysis of large amounts of quantitative features from imaging. This is based on the hypothesis that the underlying patterns at the genetic and cellular level are reflected in the imaging. Our approach is to integrate all of these sources of information to help us differentiate between these tumours. This data also feeds into mathematical models of tumour growth that may help us to understand the specific mechanisms that contribute to carcinogenesis in IPMNs. In the next article we will describe these exciting areas of research in more detail.
“This work was sponsored by the MD Anderson Cancer Moonshots program, Sheikh Ahmed Center for Pancreatic Cancer Research, and National Institutes of Health grant U01CA196403.”
Eugene J. Koay
Department of Radiation Oncology,
Sheikh Ahmed Center for Pancreatic Cancer Research, MD Anderson Cancer Center
Tel: +1 713 563 2000
ekoay@mdanderson.org
https://www.mdanderson.org/research/departments-labs-institutes/labs/fleming-koay-laboratory.html
Affiliations:
Vittorio Cristini – Center for Precision Biomedicine, Brown Foundation Institute of Molecular Medicine,
University of Texas Health Science Center at Houston (UTHealth) McGovern Medical School
Anirban Maitra – Departments of Pathology and
Translational Molecular Pathology, Sheikh Ahmed
Center for Pancreatic Cancer Research, MD Anderson Cancer Center
Annabelle L. Fonseca – Department of Surgical
Oncology, MD Anderson Cancer Center
Please note: this is a commercial profile











