Dr. Josef Penninger led an international team to investigate a drug that could stop infection in the early stages of COVID-19
This research was partly funded by the Federal Canadian government, to support the development, testing and implementation of ways to manage the pandemic. Rumours have been circulating social media platforms at the speed of light, discussing the imminence or the impossibility of a real cure. Here, we discuss the ongoing research of a trial drug that is biologically capable of preventing fatalities from Coronavirus.
How could a drug stop the early stages of COVID-19?
The answer is by closing the ‘door’ that COVID-19 uses to enter the cells of your body.
The ‘door’ is the ACE2 protein on the surface of the cell membrane.
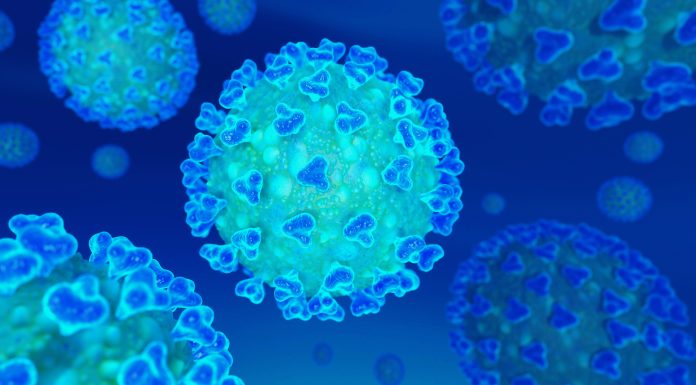
SARS-CoV-2 is the virus that causes COVID-19, which is commonly known as Coronavirus. During the last major outbreak of SARS, a similar viral respiratory illness that caused global devastation in 2003, it was Dr. Penninger and his colleagues who discovered that the ACE2 protein was the key receptor for SARS. In further research, he discovered that this protein was linked to a resultant cardiovascular disease and lung failure.
The ACE2 protein is where the spike glycoprotein of SARS-CoV-2 enters the human cell, like a ‘door’ being broken down. The world is looking for a cure – but there is no clinically proven antiviral treatment right now, or any treatment focusing on protecting the ACE2 receptor. This means that late-stage COVID-19 can be a fatal situation for those who are already experiencing other immune or lung issues.
The NHS defines antiviral treatment as: “a type of medication used specifically for treating viral infections. They act by killing or preventing the growth of viruses.”
The researchers here are not proposing a treatment that could kill the virus – they are exploring the potential of highly calculated self-defence, on a microscopic level. What if those cellular ‘doors’ were never broken down by the invading COVID-19 forces, because they were hidden or protected?
Dr. Josef Penninger, the UBC scientist leading this study, said:
“There is hope for this horrible pandemic.”
What did the research uncover?
The study found that in cell cultures, hrsACE2 inhibited the early stages of COVID-19 load by a factor of 1000-5000. The researchers grew organs of blood vessels and kidneys from stem cells, to quickly test their ideas on a functioning human being.
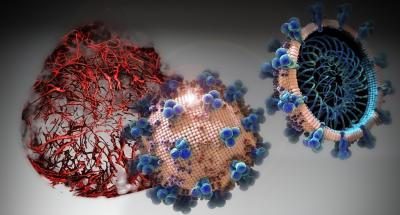
© IMBA/Tibor Kulcsar
Núria Montserrat, ICREA professor at the Institute for Bioengineering of Catalonia in Spain, said:
“In these moments in which time is short, human organoids save the time that we would spend to test a new drug in the human setting.”
The researchers showed that in these organs, the virus can directly infect and duplicate itself in the tissues of the blood vessel and kidney. This gave them valuable insight into how COVID-19 cases that are severe present with multi-organ failure, with evidence of cardiovascular damage.
It was found that clinical grade hrsACE2 reduced the infection in these engineered organs.
Dr. Art Slutsky, a scientist at the Keenan Research Centre for Biomedical Science of St. Michael’s Hospital and professor at the University of Toronto, said:
“Our new study provides very much needed direct evidence that a drug — called APN01 (human recombinant soluble angiotensin-converting enzyme 2 – hrsACE2) — soon to be tested in clinical trials by the European biotech company Apeiron Biologics, is useful as an antiviral therapy for COVID-19.”
When will APN01 be available for use?
Apeiron Biologics write that they are currently planning a clinical pilot study in China with COVID-19 infected patients, whilst “evaluating options” for further clinical development. APN01 was previously being used for Acute Lung Injury and Pulmonal Arterial Hypertension, for which the company currently have APN01 in Phase-2 clinical development. It is possible, given the existing Phase-2 level of development, that the next clinical trial for COVID-19 could automatically go to Phase-3. The length of Phase-3 clinical trials in Canada are usually one to three years, which involves around 1000-3000 patients. After that, the regulatory review can take anything between six months to two years.
However, given the global urgency, funding from Canadian government and clinical trials being held in China, it is highly likely that development of APN01 will be fast-tracked. We reached out for comment to the biotech company about possible timelines but have received no response at the time of publishing.

Penninger, professor in UBC’s faculty of medicine, director of the Life Sciences Institute and the Canada 150 Research Chair in Functional Genetics at UBC said:
“This work stems from an amazing collaboration among academic researchers and companies, including Dr. Ryan Conder’s gastrointestinal group at STEMCELL Technologies in Vancouver, Nuria Montserrat in Spain, Drs. Haibo Zhang and Art Slutsky from Toronto and especially Ali Mirazimi’s infectious biology team in Sweden, who have been working tirelessly day and night for weeks to better understand the pathology of this disease and to provide breakthrough therapeutic options.”
“The virus causing COVID-19 is a close sibling to the first SARS virus.
“Our previous work has helped to rapidly identify ACE2 as the entry gate for SARS-CoV-2, which explains a lot about the disease. Now we know that a soluble form of ACE2 that catches the virus away, could be indeed a very rational therapy that specifically targets the gate the virus must take to infect us. There is hope for this horrible pandemic.”
The findings of the study have been published in Cell.