Cannabis is the most consumed illicit drug in Europe. Latest estimates from the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) indicate that about 23 million (8%) adults (15-64 years old) used cannabis in 2022
How common is cannabis use?
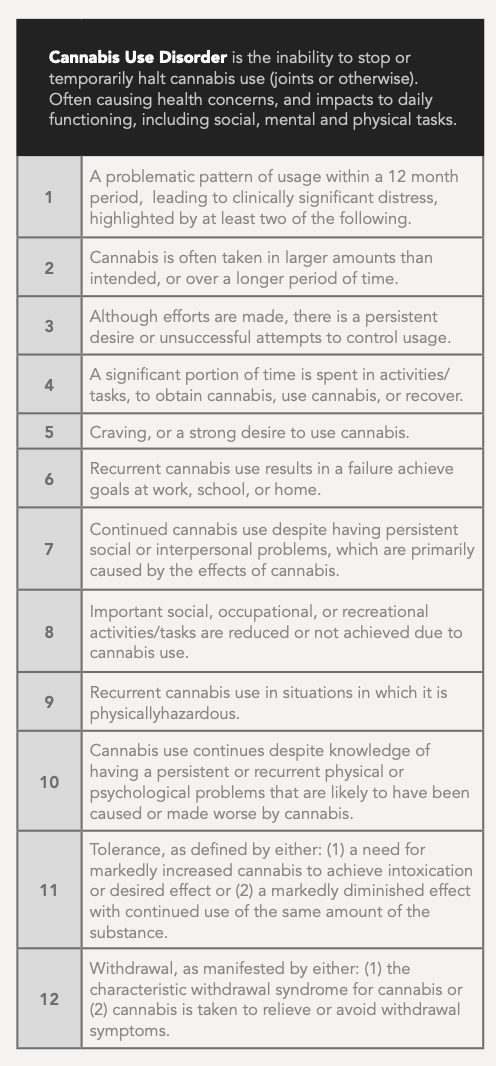
Cannabis is the most consumed illicit drug in Europe. The latest estimates from the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) indicate that about 23 million (8%) adults (15-64 years old) used cannabis in 2022. (EMCDDA, 2023) Moreover, it is estimated that 0.6% of adults in Europe have a cannabis use disorder (CUD), [See Table 1] which represents about 1.7 million people. (Manthey et al., 2021) Using this estimate, the Global Burden of Disease Study estimates that CUD in Europe is associated with 158,000,000 disability-adjusted life years (DALYs) (Shao et al., 2023). People aged 15-24 years, especially young males, are the heaviest users of cannabis, so this burden of poor health falls disproportionately upon them (Manthey et al., 2021). It is estimated that around 1.3 % of adults in the European Union (3.7 million people) use cannabis daily or almost daily.
How common is daily cannabis use among young people?
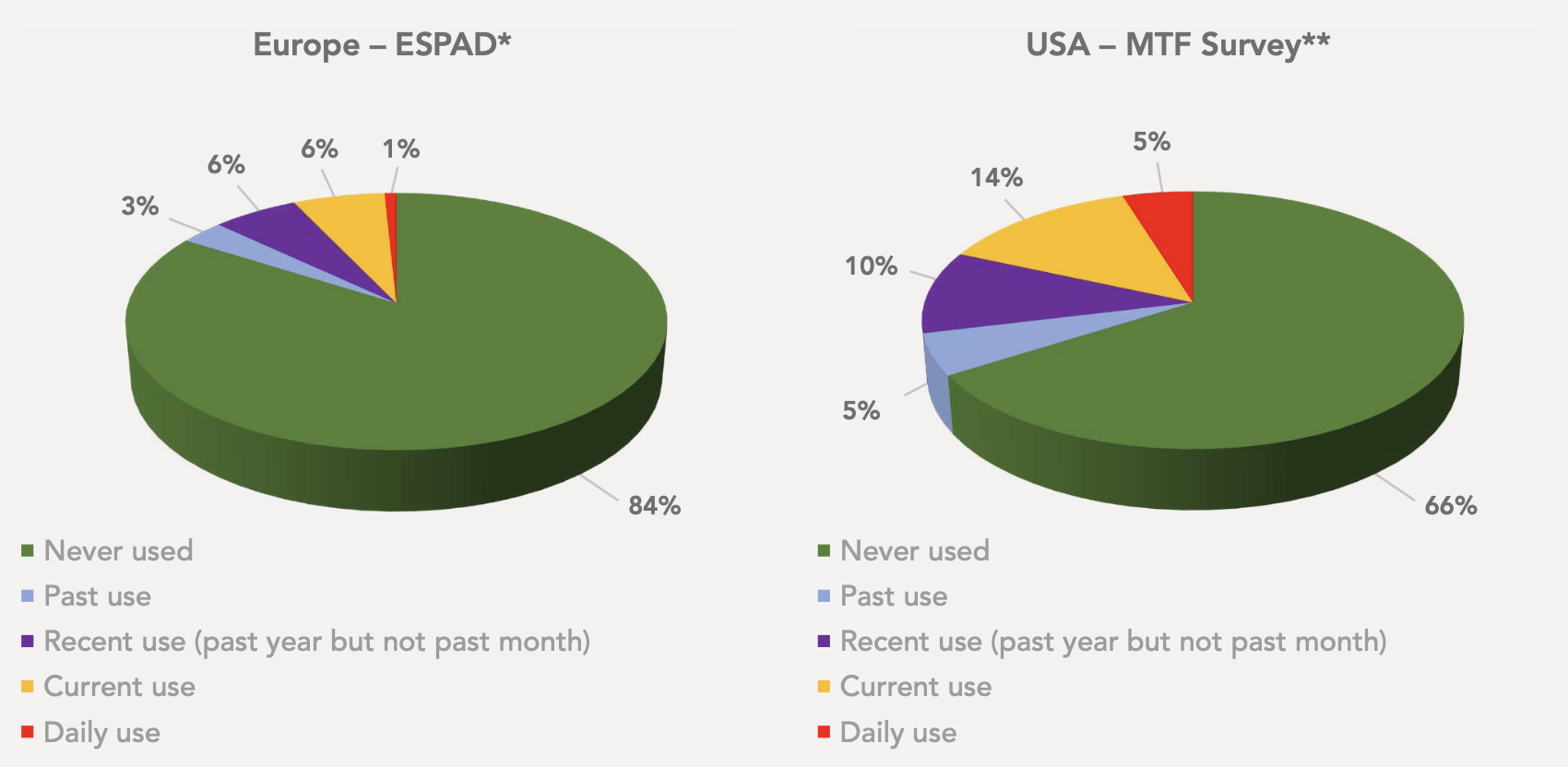
Daily cannabis use is a risk factor for the development of dependence and cannabis use disorder. It is estimated that approximately 0.8% of 16-year-olds in Europe use cannabis daily (See Figure 1). Europe has marginally increased daily cannabis use among 16-year-olds from ~0.5% in 1995 to 0.8% in 2019 (ESPAD 2020). In contrast there has been a six fold increase in daily cannabis use by 16-year-olds in USA from 0.8% 1991 to 4.8% in 2019 ((Johnston et al., 2021). The Canadian prevalence of daily cannabis use among 16 to 19-year-olds was 9% in 2020. (Health Canada, 2020).
Acute effects of cannabis use on health
In a recent European study investigating a drug-related visit to hospital emergency departments (EDs), cannabis emerged as the drug most frequently associated with presentations (Miró et al., 2023). In cases where cannabis was the only drug consumed by those under 20 years of age, the most common presenting symptoms consisted of vomiting (35%), anxiety (26%), reduced consciousness (21%), agitation (20%) and palpitations (13%) (Schmid et al., 2022). The prominence of vomiting as an issue in EDs may relate in part to cannabinoid hyperemesis syndrome (CHS) (Chocron et al., 2019; Myran et al., 2022b). This condition involves persistent intense vomiting affecting a minority of regular cannabis users.
Edible cannabis products have proliferated with legalization in the USA and Canada. These products often resemble children’s jellies, and accidental consumption can occur (Langrand et al., 2019)…(Myran et al., 2022c, Roth et al., 2022).
Cannabis may also affect attention and psychomotor functions, causing impaired driving and increased risk of accidents, including risk of injury or possibly death. (Hall, 2015; Solmi et al, 2023).
Psychoactive constituents of cannabis
Tetrahydrocannabinol (THC) is the major psychoactive component in cannabis and the cannabinoid responsible for both intoxication and adverse acute mental health effects. (Murray et al., 2016) Modern cannabis tends to have higher concentrations of THC and, therefore, is associated with a greater likelihood of mental health problems (Petrilli et al, 2022). Research findings have indicated a significant proportion of controls will develop psychotic symptoms when subjected to a sufficiently high dose of THC in experimental conditions (Murray et al., 2016).
Synthetic cannaboid receptor agonists
In 2009, synthetic cannabinoid receptor agonists (SCRAs) surfaced as a European concern, as they were legally available to be purchased and not expressly prohibited under drug laws (Smyth et al, 2020). These substances elicit similar effects to cannabis, however often more severe, with the potential for lethal ramifications in cases (Winstock et al., 2015; Potts et al., 2020; Tait et al, 2016). While SCRAs are now prohibited, they remain accessible through the black market (EMCDDA, 2021). The commercialisation of the Canadian and USA cannabis markets has led to product diversification, including edibles, extracts and vapes. Ultimately in 2022, these products have arrived in Europe, as seen in the case of hexahydrocannabinol (HHC). While several countries have banned HHC, some have allowed HHC edibles or vapes. Resulting in highlighted concerns in case reports of THC akin related risks, e.g., psychosis (O’Mahony et al., 2024).
* Data Published by EMCDDA and available at: https://www.emcdda.europa.eu/data/stats2023/tdi_en
Chronic effects of cannabis use on youth health
Dependence and addiction
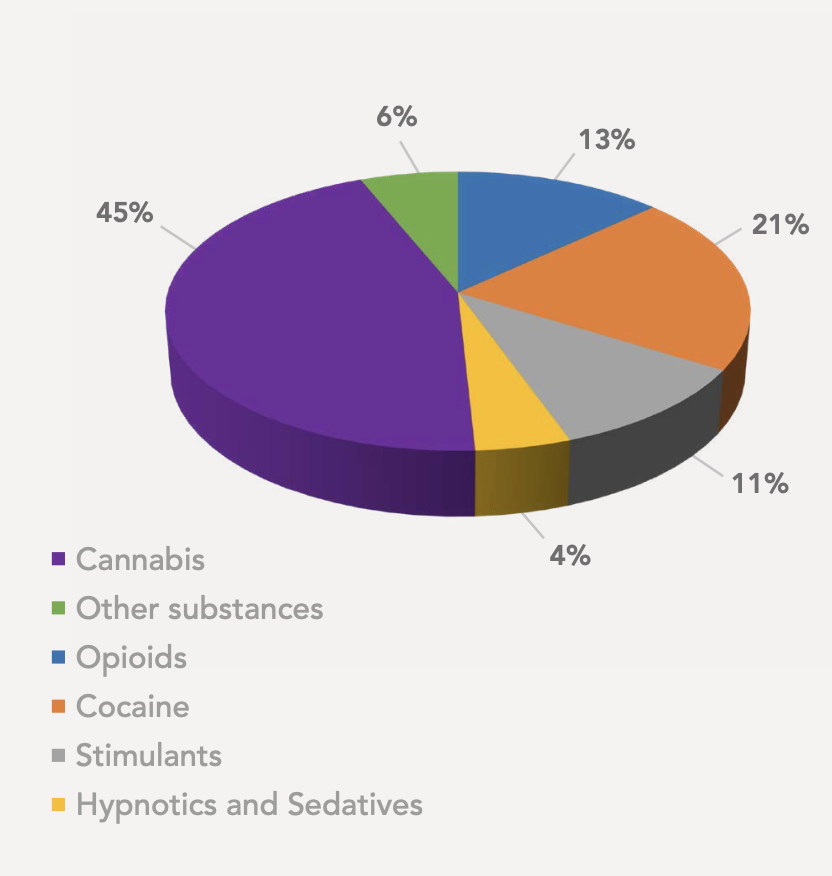
Cannabis is an addictive substance, leading to 20% of users developing cannabis use disorder (CUD), of which the most at risk are young and male (Connor et al., 2021; Leung et al., 2020; Millar et al, 2021; Volkow et al., 2014). It is estimated that one in three young people who use cannabis weekly have cannabis dependence, more often than not CUD (Leung et al., 2020). Within Europe, individuals obtaining first-time treatment for cannabis use generate the largest demand for additional service, accounting for 45% (43,000 people) (EMCDDA, 2022). European demand for such services has sharply increased by 35% from 2010-2018. (See Figure 2)
Cannabis Withdrawal Symptoms
Cannabis dependence can result in withdrawal symptoms (Gorelick, 2023, Connor et al., 2022):
- Irritability, anger or aggression
- Nervousness or anxiety, or depression
- Sleep difficulty or restlessness
- Decreased appetite or weight loss
Mental health harms
Regular cannabis use is associated with adverse effects on mental health, such as psychosis, mania, depression and anxiety disorders (Murray et al, 2016; Gobbi et al, 2019; Solmi et al, 2023; Myran et al, 2023b; Gibbs et al, 2015; Kedzior et al, 2014, Gorelick, 2023, Myran et al, 2024). Adolescent and young adult cannabis use raises the greatest concern from a mental health perspective, as it is associated with a higher risk of suicide attempts and suicidal thoughts than older adult use (Gobbi et al., 2019; Han et al., 2021; Zahra et al., 2020). In an Australian study of 550 deaths in which cannabis was implicated, 25% of the deaths were by suicide (Zahra et al., 2020).
Cannabis and psychosis
There is now strong evidence that cannabis use is causally related to the subsequent development of psychotic illnesses such as schizophrenia (Power et al., 2023). An estimated 12% of first-episode psychosis cases are associated with high-potency cannabis, yet the use of cannabis at any potency increases the risk of psychosis development (Di Forti et al., 2019). A European study has estimated that 30% of schizophrenia cases in young males could be related to a pre-existing cannabis use disorder. (Hjorthøj et al., 2023).
Effects of youth cannabis use on brain structure and function
Adolescent cannabis use is associated with a decline in IQ of between 2-8 points and is evident in later adulthood (Meier et al., 2012, Meier et al., 2022, Power et al., 2021). Cannabis use among young people is also associated with volumetric changes in white matter in longitudinal brain imaging studies. (Owens et al., 2022, Albaugh et al., 2021, Albaugh et al., 2023). One study reported significant unexplained grey matter volume differences among 14-year-olds who reported extremely low levels of cannabis use. (Orr et al., 2019). The endo-cannabinoid system is involved in guiding key aspects of the delicate process of brain maturation, which occurs in adolescence and young adulthood. (Lubman et al., 2015). It is possible that stimulation of the endo-cannabinoid system by cannabis use during youth brain development may adversely affect these maturational processes. These changes may not be entirely reversible.
Effects of youth cannabis use on physical health
Smoking cannabis contains many of the same toxins and carcinogens as tobacco smoke and has been linked to risk of chronic bronchitis (American Lung Association, 2022; California Environmental Protection Agency, 2009; Canadian Lung Association, 2018). There is evidence of an association between cannabis use and non-seminoma testicular cancer (Hoch et al, 2019; Callaghan et al, 2017; Gurney et al, 2015). Cannabis use has been linked to an increased risk of heart attacks, atrial fibrillation, heart failure and stroke. (Page et al., 2020; Bahji et al, 2023; Testai et al., 2022). Daily cannabis users are 25% and 42% more at risk of a heart attack or stroke, respectively, compared to non-cannabis users (Jeffers et al, 2024).
Effects of youth cannabis use on educational achievement
Longitudinal studies have provided evidence of negative psychosocial consequences of regular cannabis use in early or mid-adolescence, such as more frequent school dropouts and lower subsequent attainment of university degrees. (Boden et al, 2020, Ferguson et al, 2015, Danielsson et al, 2015, Volkow et al, 2014).
Cannabis use and harm to others
Cannabis use is often considered to be just a matter for the individual themselves but there are also potential public health impacts by means of “harm-to-others”. (Boury et al., 2022;
Fischer et al, 2023).
- Driving:
- Cannabis intoxication impairs driving ability and provides a two-to-three fold increased risk of a road traffic collision (Hall, 2015; Solmi et al, 2023).
- Violent behaviour:
- There is growing evidence that cannabis may contribute to violent behaviour, for instance, a two- to three-fold increased risk of intimate partner violence (Daldegan-Bueno et al., 2022; Dellazizzo et al., 2020a; Dellazizzo et al., 2020b). In patients with psychosis, ongoing cannabis use is associated with increased risk of violence. (Dugré et al., 2017, Beaudoin et al., 2023). Family members often experience the anger and irritability of young cannabis users in the home with adverse mental health effects on siblings and parents. (Connor et al., 2022)
- Accident poisonings:
- Children may experience accidental poisoning from cannabis-based edible products which belong to parents or older siblings, as many of these products are often manufactured to look like children’s sweets. (Langrand et al., 2019).
- Effects on the developing fetus:
- There are risks if cannabis is used during pregnancy. (Bandoli et al., 2023; Solmi et al, 2023) These can include low birth weight and pre-term delivery. (Marchand et al., 2022, Dodge et al., 2023, Metz et al, 2023) There is growing evidence of adverse neuro-psychological impacts on children exposed to cannabis in utero, e.g., memory, impulse control, and problem-solving. (Baranger et al., 2022, Paul et al., 2021, Sharapova et al, 2018).
The effects of changes in drug policy on youth cannabis use
Effects on cannabis use trends
Over the past 30 years, cannabis policy has created serious international debate, with many countries liberalizing their laws. This debate sparked with provision of greater access to cannabis for purported “medical use”, most notably within US states (mid-1990s) and Canada (2001). This has been followed by legalization for more general adult use and the growth of the legal cannabis industry in North America (Connor et al., 2021). Although the legalization of cannabis in Canada was accompanied by political assurances to prevent access by children, enhance public health outcomes and eliminate the illicit market (Boury et al., 2022), it appears not to have achieved these promised aims.
Canadian and American data has indicated that youth cannabis use has not declined (See Figure 1), (Smyth and Cannon, 2021). There is evidence for an increase in adolescent Cannabis Use Disorder rates in US states that have legalized cannabis (Cerdá et al., 2020; Imtiaz et al, 2023a). There is also emerging evidence of increases in rates of intensive and harmful use in legal locations. (Imtiaz et al., 2023b, Hasin, 2023, Kilmer et al., 2022) The US Household Survey indicates that the prevalence of daily use by adults increased 10-fold from 1992 to 2021, while past year use doubled. Daily use by adults in Canada increased six-fold across the period of cannabis policy liberalization and ultimate legalization, from 2000 to 2019.(Imtiaz et al., 2023b). There was a significant acceleration in daily and harmful use patterns following the announcement of Government plans to legalize in Canada, and this increased further following actual legalization. (Imtiaz et al., 2023b)
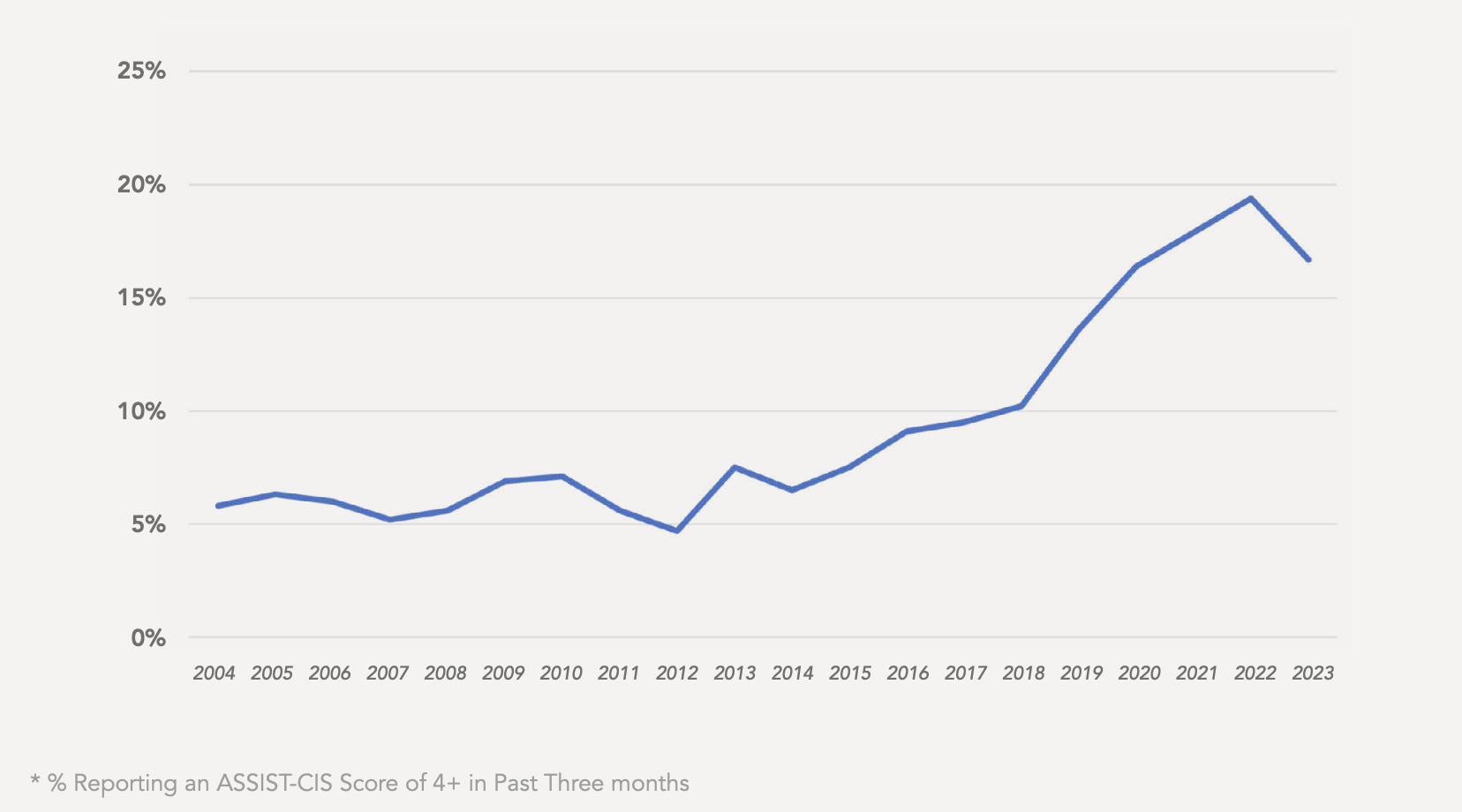
The Ontario Canada CAMH Monitor Survey has been measuring patterns of drug use for over 20 years, utilising a screening tool to identify people with a high pattern of cannabis use and trends from 2004-2023 (See Figure 3) (Nigatu & Hamilton, 2023). In 2004-2015 problematic cannabis use averaged 6.2%, but across the two most recent years (2022-23), the average is now 18%. Problematic cannabis use now stands highest in younger adults (aged 18-29 years), where one in four young adults self-report a moderate to high risk pattern of cannabis use.
Effects of changes in drug policy on cannabis health effects
The commercialization of cannabis has been associated with a significant increase in cannabis- related emergency department visits, as noted by various studies (Myran et al., 2022b, Myran et al., 2022a, Wolf et al., 2020, Myran et al., 2022c). Cannabinoid Hyperemesis Syndrome presentations within Canadian EDs were investigated, reporting a 13-fold increase in presentations between 2014-2021. Cannabis-induced psychosis presentations also saw a two-fold increase in presentations between 2015-2019 (Callaghan et al., 2022). In Canada & Colorado, research has suggested that cannabis-impaired drivers appear to be involved in more crashes, injuries and fatalities following legalization (Lane and Hall, 2019, HIDTA, 2019, Brubacher et al., 2022, Myran et al., 2023c). There has been a consistent pattern of increases in cannabis-related paediatric presentations to emergency departments in locations relating to the ingestion of cannabis-related products (Callaghan et al., 2023; Myran et al., 2022c; Ryan, 2021; Roth et al., 2022 Yeung et al., 2021).
Medical profession concerns
In light of the evidence that cannabis legalization has generally negative impacts on public health a growing number of international medical professional organizations have publically argued against legalization. In 2023, the Australian Medical Association (2023) said that “cannabis use can have a range of negative health impacts” and concluded that they are “concerned that if cannabis were legalised for recreational purposes, it may increase health and social-related harms”.
The Standing Committee on European Doctors (CPME, 2023) also issued a statement on cannabis in late 2023. They said: “European doctors warn that cannabis is a hazardous and addictive drug and a serious public health concern, and therefore discourages cannabis use.” They state that they “strongly oppose further legalization across Europe as the weight of current evidence indicates that legalization adds to health harms across the population.” In its updated statement on cannabis in 2023, the American Medical Association (AMA, 2023) says that it “(1) believes that cannabis is a dangerous drug and as such is a serious public health concern; (2) believes that the sale of cannabis for adult use should not be legalized”.
Summary
Cannabis is the most widely used illegal drug among youth globally. Its use is far from benign. It is associated with significant adverse health effects. Cannabis features with increasing and surprising frequency in acute presentations to emergency departments. Cannabinoid hyperemesis syndrome is an emerging phenomenon in all locations where cannabis use is increasing. The acute and chronic mental health impacts are a major area of cannabis-related health concern. There is strong evidence linking youth onset cannabis use to psychosis, to decline in IQ and subsequent suicidal behavior. About one in three young people who use cannabis regularly will develop a significant cannabis use disorder. Cannabis is now the primary driver of demand for addiction treatment amongst youth across Europe.
The increase in cannabis-related harm appears related to an increase in the prevalence of users, an intensification of use among established users and an increase in the potency of cannabis itself. The move towards legalization and commercialization in some countries only appears to have increased the harm for young people. Public health solutions are urgently needed, such as improved public information on the hazards and risks of cannabis, universal and targeted prevention initiatives and improved treatment access for those with cannabis use disorder.