Arun Swaminathan MD, Assistant Professor of Neurology and Epilepsy at the University of Nebraska Medical Center, considers the importance of improving infrastructure and management of epilepsy research
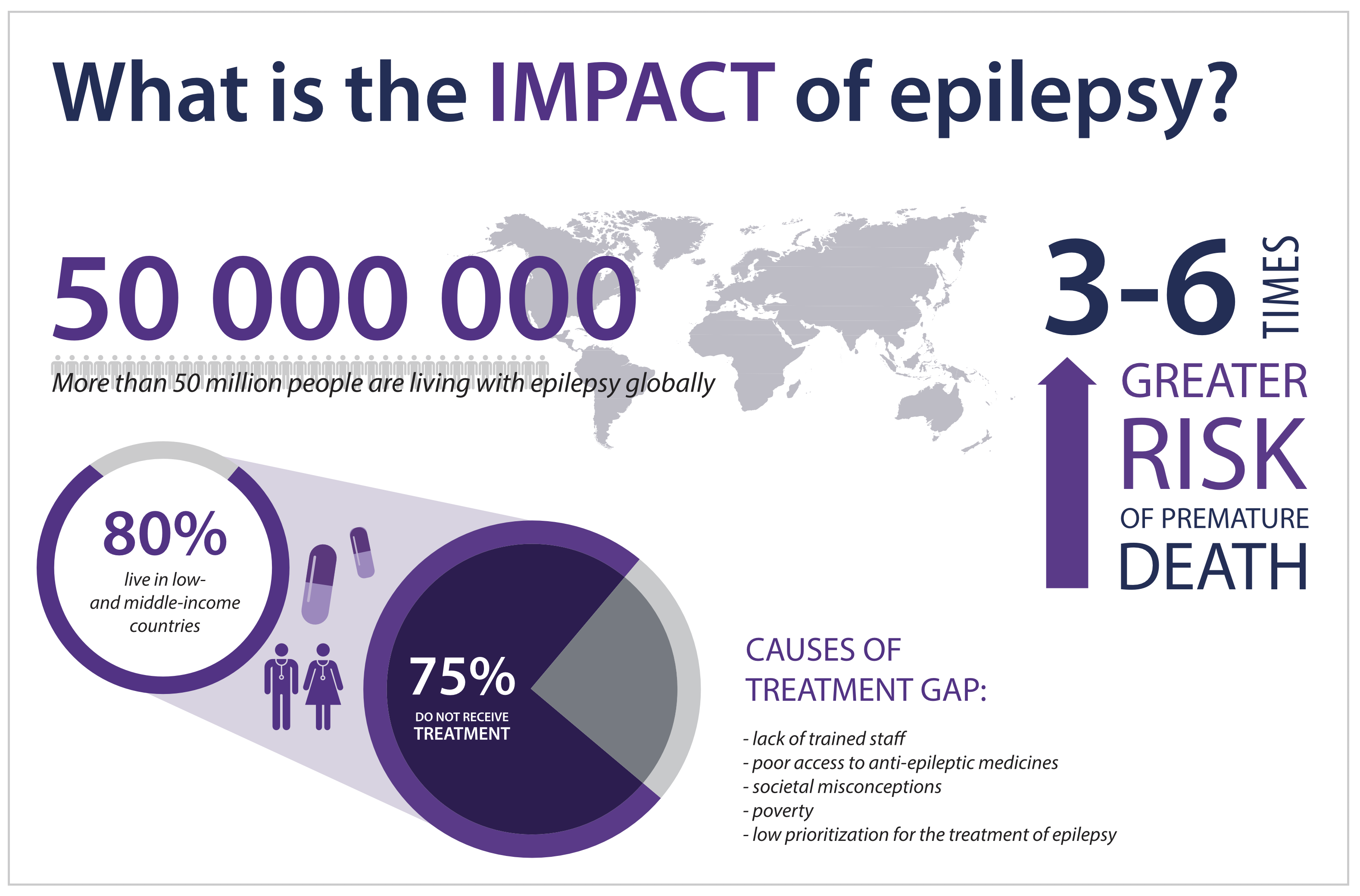
Epilepsy remains a common condition worldwide with an estimated prevalence of 50-65 million people1. A significant number of years are lost due to morbidity and mortality from uncontrolled epilepsy. The effects of uncontrolled epilepsy are noted to be more devastating in socially and financially disadvantaged populations and countries[1]. Diagnosis and treatment of epilepsy remain ongoing challenges in developing nations due to social, financial and cultural limitations, while developed nations continue to struggle with developing newer techniques to define causation and improve medical and surgical interventions for epilepsy[2].
Medical management represents the first line of treatment for epilepsy and 70% of patients will be controlled on 2-3 anti-seizure medications[3]. Patients in developing nations are unable to spend up to 1$ a month for their medications making affordability a major impediment in treatment1. The availability of newer drugs has not significantly improved seizure control, despite decreasing medication interactions and side effects, in patients from developed nations[4]. These findings highlight the need for better anti-seizure medications, along with improving affordability and access to these medications across the world. Better understanding of the causation of epilepsy would enable the development of better medications and improve outcomes, thus highlighting the urgent need for increase in research and infrastructure for the management of epilepsy.
Surgical management of seizures represents the next step in treatment after failure of medications. About one-third of epilepsy patients will be refractory to medications and qualify for surgical evaluation[3]. Availability of advanced testing, accessibility to facilities and specialists that offer these evaluations and cost of evaluation and surgery are often the limiting factors for surgical evaluation for these patients[2].
Patients in many developed countries may not receive a timely surgical evaluation due to difficulty of access and the tendency to maintain status quo using medications by trying all available medications before declaring failure of medications. Worldwide estimates suggest that 10.1 million patients with epilepsy may be surgical treatment candidates, and 1.4 million new surgically treatable epilepsy cases arise annually[5]. Many centres have established low-cost approaches in resource limited settings to facilitate better care[6]. These numbers and factors underscore the importance of increased investment into diagnosis, treatment, and research in epilepsy to improve accessibility, affordability and outreach to patients to improve outcomes in management of epilepsy.
Studies have focused on the direct financial implications of epilepsy on patients and healthcare systems. Analyses in the USA have estimated that costs of management vary from 8,000-50,000$ per patient with epilepsy, depending on severity of the condition and acuity of care[7]. European statistics estimate systems expenditure to approach 15 billion euros for a single year with cost per patient ranging from 2,000-12,000 euros[8]. Numbers from Asia, Africa and Latin America are more limited due to lack of collected data and paucity of resources from the personal and systems point of view. Increased investment into research and care and improved utilization of resources would go a long way towards improving efficacy and accuracy of treatments and research. Moreover, these numbers only look at the direct financial costs for patients and systems and not the social and cultural costs for patients. WHO studies estimate that epilepsy accounts for 180-200 disability adjusted life years (DALYs) per 100,000 patients[1]. Socio-cultural costs from epilepsy remain high in patients from developing nations due to limited awareness and resulting ostracization from employment and society in general limiting physical and mental health along with social and financial wellbeing.
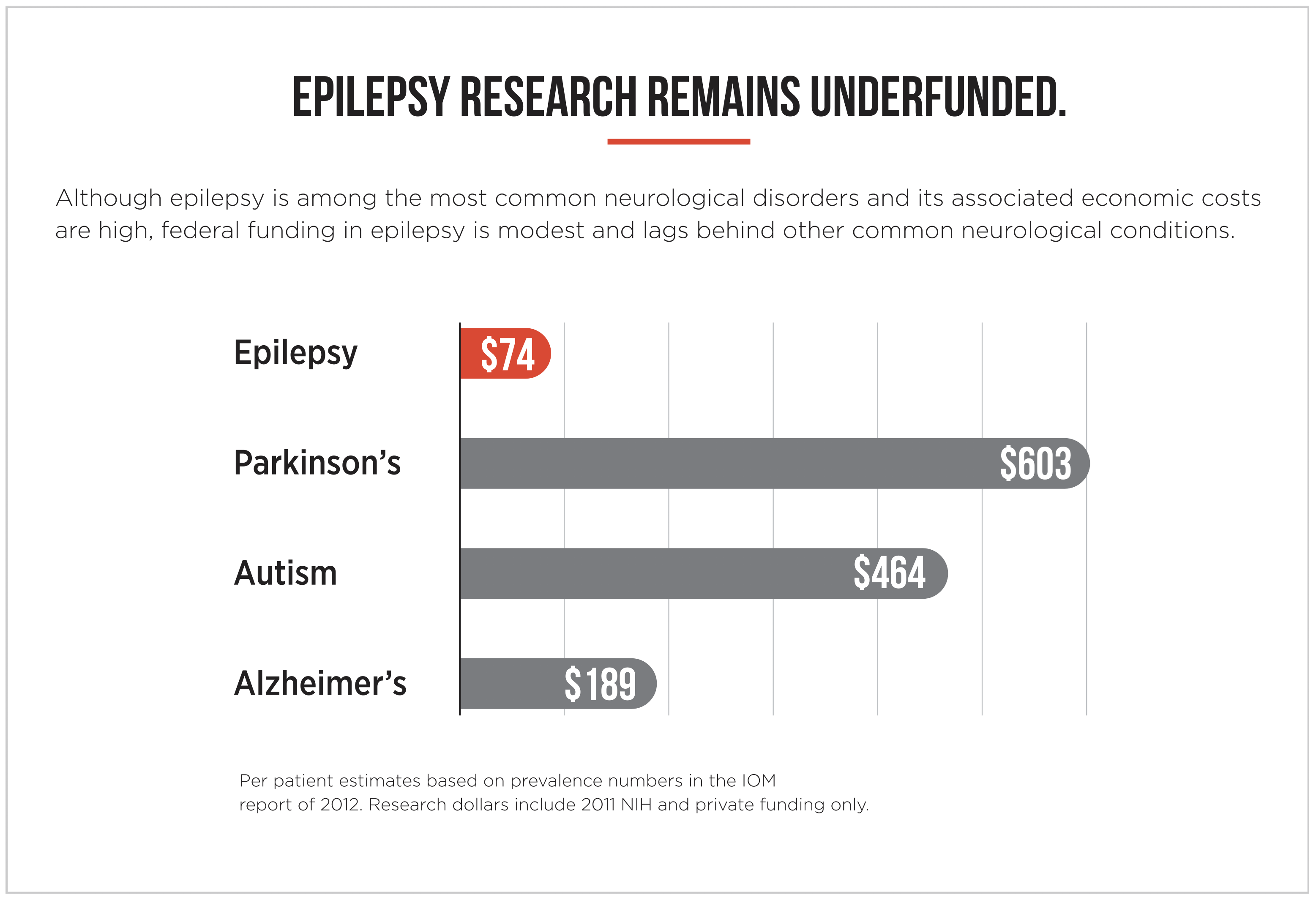
Financial estimates of funding for epilepsy research show that monetary allocations for it have been woefully poor. NIH funding for epilepsy research in the USA lags behind support for other conditions like stroke, dementia and even less prevalent conditions like multiple sclerosis and motor neuron disease[9]. The reasons for this disparity are diverse and include less awareness for epilepsy and greater publicity for many of these conditions, among others9. Numbers from other parts of the world are equally discouraging, if not worse.
All the points highlighted above strongly support the need for increased investment into epilepsy research and management. Resource rich and resource limited nations alike need to step up efforts to improve access to care and investment in research and drug development to account for the high prevalence and socioeconomic impact of epilepsy across the world. If November is Epilepsy Awareness Month, then we need to ensure that the 2020s become the Decade of Epilepsy Research to combat this worldwide scourge and improve the lives of millions globally.
References
1 GBD 2016 Epilepsy Collaborators. Global, regional, and national burden of epilepsy, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 [published correction
appears in Lancet Neurol. 2019 May;18(5): e4]. Lancet Neurol. 2019;18(4):357-375.
2 Newton CR, Garcia HH. Epilepsy in poor regions of the world. Lancet. 2012; 380:1193–1201.
3 Kwan P, Brodie MJ. Early identification of refractory epilepsy.
N Engl J Med. 2000 Feb 3;342(5):314-9.
4 Chen Z, Brodie MJ, Kwan P. What has been the impact of new drug treatments on epilepsy? Curr Opin Neurol. 2020 Apr;33(2):185-190.
5 Vaughan KA, Lopez Ramos C, Buch VP, Mekary RA, Amundson JR, Shah M, Rattani A, Dewan MC, Park KB. An estimation of global volume of surgically treatable epilepsy based on a systematic
review and meta-analysis of epilepsy. J Neurosurg. 2018 Sep 1:1-15.
6 Jukkarwala A, Baheti NN, Dhakoji A, Salgotra B, Menon G, Gupta A, Prakash S, Rathore C. Establishment of low cost epilepsy surgery centers in resource poor setting. Seizure. 2019 Jul;69:245-250.
7 Begley CE, Durgin TL. The direct cost of epilepsy in the United States: A systematic review of estimates. Epilepsia. 2015 Sep;56(9):1376-87.
8 Pugliatti M, Beghi E, Forsgren L, Ekman M, Sobocki P. Estimating the cost of epilepsy in Europe: a review with economic modeling. Epilepsia. 2007 Dec;48(12):2224-33.
9 Meador KJ, French J, Loring DW, Pennell PB. Disparities in
NIH funding for epilepsy research. Neurology. 2011 Sep 27;77(13):1305-7.
*Please note: This is a commercial profile











