Rick Goodman, Research Professor for the Food Allergy Research and Resource Program, University of Nebraska, discusses food allergy risk assessments for new foods in different countries, including GMOs and novel foods
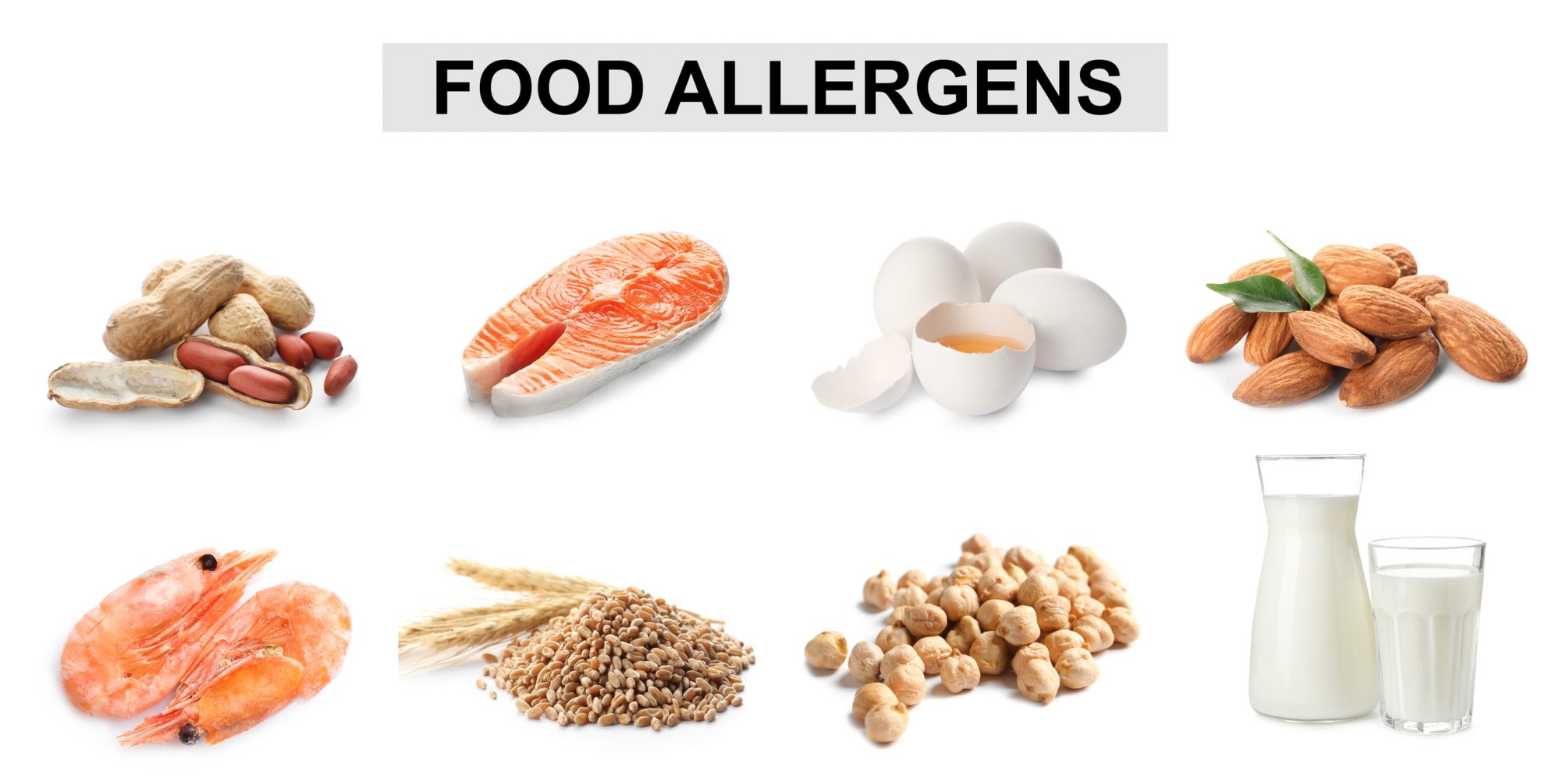
The prevalence of food allergy in most countries is apparently increasing, although prevalence and severity for most consumers is not clear. Food allergy has been estimated by knowledgeable experts for some countries and commonly allergenic foods. There are clear differences in the prevalence and major allergen sources in many countries with most of it available from North America (USA and Canada) parts of the European Union (primarily through Europrevall studies) from Japan, Australia and parts of India and China. Food allergy concerns play a major role in the acceptance and regulation of many new food products.
Diagnosis of food allergy and celiac disease is a health concern of growing proportions
Accurate diagnosis of food allergy and celiac disease requires knowledge by doctors. Telling allergic consumers or celiac patients how to stay safe requires knowledge by the doctor, the patient, food companies and restaurants. What are the symptoms of food allergy? Rapid onset of symptoms within minutes to an hour or two for IgE mediated food allergy. Symptoms ranging from tingling in the mouth, to angioedema, hives, vomiting, diarrhoea and asthma can be symptoms. There are other causes for each of those symptoms, but if they frequently or always occur after eating the same food, it is likely food allergy. Furthermore, the responsibility of labelling packaged foods to allow allergic consumers to avoid the cause of their disease is essential for food safety, and accepting enhanced GMO crops for food production is important. Food safety regulatory authorities, clinicians and patients should all have some knowledge of the foods that cause reactions and the types of foods that might have ingredients from their allergenic source.
The type of foods that cause allergy differs markedly between people and cultures. The highest prevalence of food allergy to different sources also differs between adults and children and depends markedly on food ingestion patterns. In the USA food allergy prevalence was predicted for prevalence for children and adults to the most common allergenic sources and is listed based on predictions from careful interviews, serum IgE testing, skin prick testing and food challenges. The groups were in New York City and Baltimore in the USA and the population’s typical consumers of U.S. foods. Allergy to cow’s milk was estimated to be in children and in adults (Sampson, 2005). The numbers are reported here as the percent of both groups in the population (children/adults) for cow’s milk (2.5%/0.3%), chicken eggs (1.3%/0.2%), peanut (0.8%/0.6%), tree nuts (common tree nuts combined 0.2%/0.5%), finned fish (0%/0.4%) and shellfish (0.1%/2.0%). A follow-up paper in 2010 showed the same numbers but added prevalence for wheat and soy (0.4%/0.3%), as well as sesame seeds (0.1%/0.1%) by Sicherer and Sampson (2010). That allergy group in New York and their collaborators in Baltimore are referral centres and see many hard to diagnose and severe allergic subjects. Based on their data and that of several other centres in the U.S., packaged foods containing proteins from those sources (milk, eggs, peanuts, tree nuts, crustacean shellfish, fish, soybeans and wheat) must be clearly labelled in plain English terms for the source being in the food based on a 2004 federal law). Canada uses the same list and has added mustard. The USA and Canada are also now going to add sesame seed sources that require food labelling in 2022. Similar allergenic sources are recognised in Europe but they a few more including celery (celeriac, the root) mustard, sesame and lupine (FARRP website; and EU Regulation 1169/2011).
Differences in reports of food allergy and celiac disease prevalence can be puzzling
Data are potentially skewed in each country by differences in food use patterns but also in biases of clinical practices and the availability of appropriate diagnostic tools looking at country reports described by Conrado et al., (2021) from a systematic review of published reports across the globe of food anaphylaxis. Publications from some countries show no or limited prevalence of anaphylaxis to major allergen sources while in other countries the numbers are very high. But reporting is not very uniform.
The accuracy of diagnosis is clearly important for the individual, however these variations might also be due to:
- Differences in food patterns.
- Reports may be inaccurate.
- Built in environmental differences in countries such as very low reports of allergy to cow’s milk in Morocco’s very dry climate. Although that is a major allergenic source in most countries and especially in children, the reports from Morocco show high prevalence to chicken egg, which is very common in most countries as a dominant allergenic source.
- Economic reasons may also reflect differences due to food preferences or the use of medical practices.
- Communication and the availability of diagnostic tools including high quality skin prick test extracts or laboratory tests which differ between countries.
- Doctors can also be swayed by their peers and their clients.
- Social media influence or comments by friends and inaccurate advertisement that may mislead consumers.
- Additionally, some doctors are not adequately trained in food allergy during medical school (Kim and Sicherer, 2011; Shaker and Ventor 2016).
Misinformation can stand in the way of good nutritional health of infants and children (Brown et al. 2020). As noted, some pregnant or nursing mothers avoid the consumption of cow’s milk which is a major source of calcium and of total digestible protein because of misleading fears of giving their child food allergy (Brown et al., 2020). In rare cases, a mother’s milk may contain sufficient amounts of some proteins from cow’s milk to elicit symptoms in the most sensitive cow’s milk allergic infants, but that is rare. Importantly the infants have critical needs for proteins, lipids, carbohydrates, minerals and vitamins that impact their health as they grow, and this avoidance behaviour may rob the infant of essential nutrients.
Celiac disease (CeD) is similar to food allergy by being specific to a food source: wheat, barley, rye and related grass grains that contain specific gluten proteins that are needed for easy production of bread. Antigen-presenting cells process glutens and attached peptides to specific MHC class II receptors for activation of CD4+ T cells that cause the autoimmune disease. Symptoms usually occur over hours and days after ingesting gluten rather than the minutes needed for IgE mediated food allergy reactions (Lindors et al., 2019). CeD is genetically restricted to specific antigen receptors, but the prevalence is 1.3% to 2% of consumers while the MHC types are present in 30% of all people, making it hard to diagnose. Avoidance of those grains is difficult as grain proteins are included in many foods and now many groups are searching for therapies (Kovela et al., 2021). Nearly 10% of consumers in the USA believe they have CeD or complain of symptoms that are probably related to fructan sugars in wheat that are metabolised by bacteria in the intestine (Lindors et al., 2019). There is a growing demand for gluten-free foods which are a challenge to produce in the same food format that could have wheat and relatives, as much less than one one-hundredth of a gram of gluten may cause a disease episode in those with severe CeD.
Beyond diagnosis, food safety and acceptance
Misinformation about food allergy, CeD and the safety of new food crops including genetically modified organisms has stalled regulatory bodies in many countries and blocked public acceptance of many food sources of products that have been accepted in the USA and some other countries. That includes decisions about GMOs in most countries of the European Union, most countries in Africa and Asia as well as some countries in Southern and Central America. It also increases the demand for products claiming to be “allergen-free”, “gluten-free” and “Non-GMO.” The messages are often quite misleading, and they imply that foods with allergens, gluten or some GMO ingredients are unsafe for everyone. Yet food allergy and celiac diseases are relatively rare (1% to 10% and ranging in severity) and spread across a wide variety of food sources. The severity is not well documented in reports of allergy or celiac disease. In 25 years of consuming a variety of GMO crops in the USA, there are no documented cases of harm from consuming GMOs. On the contrary, several GMOs lead to reduced environmental contamination of chemical pesticide and some reduction in mycotoxins in certain food products. GMO safety evaluations and testing are well documented in the USA and reviewed in countries that accept those products including Australia, Canada, Japan, Korea and Taiwan. Food labelling laws in many countries provide information for those at risk of specific allergies to the named primary allergen source, and for those with CeD to avoid foods above a reasonably safe minimum of gluten (20 ppm on a weight of gluten to food basis). Concerns of food allergy risk assessment have caused common confusion and rejection of GMOs in many societies. Yet the GM sources must be evaluated using scientifically defensible evaluations established by the CODEX Alimentarius Commission in 2003. The acceptance of many new or novel food products such as mealworms in the EU has also faced challenges and continues to do so in the USA. Yet insects similar to mealworms have been consumed safely in some Asian countries for centuries. A small number of people in China, where the consumption of silkworm pupae is common, have allergies to the silkworm but those allergies are easy to diagnose and the food is easy to avoid (Zhao et al., 2015). The common food safety risk from many novel products is the unintentional introduction of a hazard such as microbial, fungal or algal contamination in the case of pond-grown algae, insect cultures or unsanitary slaughter facilities. Those hazards potentially affect everyone, not just those with some allergy or CeD.
At this time of global warming, increasing populations and increasing demands for high-value foods such as beef, shellfish and exotic fruits we need to focus on science. In many cases, food production can be increased by genetically modified crops, especially in areas with marked insect pest pressure, bacterial and fungal diseases or in areas where plants are susceptible to drought. People in most countries struggle to produce sufficient healthy food for our dietary needs. Misplaced concerns can block the introduction of foods from new sources that have high protein content such as cultured insects or different species of algae or fungi. Those products may be beneficial in reducing land use and input requirements for major protein sources of meat and milk, and from major grain crops. Miscommunication or inaccurate communication can also lead to consumer rejection of products that are demonstrated to be safe food sources.
In some African countries, specific GM crops can be useful to produce insect-resistant cowpea that is often consumed by storage beetles and other useful crops (Barrero et al., 2021). Some GM maize is resistant to insects, including Fall Armyworms that managed to migrate to Sub-Saharan Africa from the Caribbean, South or Central America before 2016 and have spread across Africa into Asia and are now in Japan and Australia (Goodman and Huesing, 2020). A GM banana was developed in Africa that is resistant to bacterial blight (Goodman 2021). Another was developed in African potatoes that is resistant to Phytophthera infestans, the blight that caused the Irish potato famine in the 1800s (Ghislain, et al., 2021). Golden Rice is a nutritionally enhanced rice with high levels of beta-carotene due to the insertion of two genes from common and safe sources, at sufficient levels to produce sufficient vitamin A in the human body to provide immunity to many diseases and prevent visual loss (Datta et al., 2003; Kettenburg et al., 2018). Sometimes the personal definitions of “good” and “bad” foods and products get in the way of science. Those GMO products were developed through public-private partnerships to allow sufficient safe food production to really help feed people with nutritious products in developing countries. Many of the GM products are or will be provided to smaller holder farmers without technology fees. Yet it seems regulators in many African and Asian countries are slow to approve of the use of varieties even though they are approved in other countries.
Food safety evaluations for risks of allergy and CeD
There can be a balance of food safety, food security, fairness and economic stability. There is a guideline for evaluating the safety of GMOs and similar procedures have sometimes been used for novel foods (CODEX, 2003). But in 2021 we need to balance our increased knowledge of science (expansion and diversity of allergens, evolutionary conservation) and the desire for zero risks of allergy or CeD from foods. The source of the proteins or novel foods and history of allergy or CeD is a top consideration. Bioinformatics matches to allergens and CeD proteins are the next top priority along with searches of the scientific literature for risks. Our recent bioinformatics paper demonstrates that many genes and corresponding proteins are highly conserved in evolution. This brings to question the criteria of just over 35% identity covering 80 amino acids as a plausible pairing for allergic cross-reactivity. Many allergens listed in www.Allergen Online.org and other sequence data-bases are highly conserved minor allergens from fungi, plants and animals.
Conservation of function is high, but evidence of shared allergy or cross-reactivity is lacking. Proteins that have high identities to human proteins are unlikely to cause allergies as they should be well-tolerated due to immune recognition that makes our proteins safe. The identity levels for diverse protein types should be established for criteria of risk. When new proteins in GMOs or novel foods do not share a high identity to major allergens from peanuts, allergenic tree nuts and the major allergens from cow’s milk, chicken eggs, crustacean shellfish, finned fish they are unlikely to cause risks of allergy. If the new proteins do not have exact matches to gluten peptides in our Celiac Database with www.AllergenOnline.org, they are unlikely to trigger CeD. And there are no methods that can predict the ability of totally new proteins to sensitise humans. These practices can provide a safety screen for the new products.
References
- Abdelmoteleb M, Zhang C, Burey B, Kozubal M, Griffiths H, Champeaud M, Goodman RE. (2021). Evaluating potential risks of food allergy of novel food sources based on comparison of proteins predicted from genomes and compared to www.allergenonline.org. Food Chem Tox 147:111888. doi: 10.1016/j.fct.2020.111888.
- Barrero JM, MacKenzie DJ, Goodman RE, Higgins TJV. (2021) A biotech shield for cowpea against the major insect pests. OpenAccessGovernment. https://www.openaccessgovernment.org/major-insect-pests/111590/.
- Brown K, von Hurst P, Rapson J, Conlon C. (2020). Dietary choices of New Zealand Women during Pregnancy and Lactation.Nutrients 12(9):2692. Doi: 10.3390/nu12092692.
- Conrado AB, Patel N, Turner PJ. (2021). Global patterns in anaphylaxis due to specific foods: A systematic review. J Allergy Clin Immunol 148:1515-1525.
- Datta K, Baisakh N, Oliva N, Torrizo L et al. (2003) Bioengineered ‘golden’ indica rice cultivars with beta-carotene metabolism in endosperm with hygromycin and mannose selection systems. Plant Biotechnol J 1(2):81-90.
- Kettenburg AJ, Hanspach J, Abson DJ, Fisher J. (2018). From disagreements to dialogue: unpacking the Golden Rice debate. Sustaain Sci 13(5):1469-482.
- Kim JS, Sicherer SH. (2011). Living with food allergy: allergen avoidance. Pediatr Clin North Am 58(2):459-470.
- Kivela L, Caminero A, Leffler DA, Pinto-Sanchez MI, Tye-Din JA, Lindfors K. (2021). Current and emerging therapies for coeliac disease 18:181-195.
- Ghislain M, Goodman RE, Barekye A. (2021). Defeating late blight disease of potato in sub-Saharan Africa. OpenAccessGovernment. https://www.openaccessgovernment.org/late-blight-disease/108180/.
- Goodman RE. (2021). GE crops: biotech and novel food safety conflicts. OpenAccessGovernment. https://www.openaccessgovernment.org/ge-crops-biotech-and-novel-food-safety-conflicts/111343/.
- Goodman RE and Huesing J. (2020). African and Asian Agriculture. OpenAccesssGovernment. https://www.openaccessgovernment.org/2021-african-and-asian-agriculture/98500/.
- Lindfors K, Ciacci C, Kurppa K, Lundin KEA et al. (2019). Coeliac disease. Nat Rev Dis Primers 5(1):3. Doi: 10.1038/s41572-01809954-z.
- Sampson HA. (2005). Food allergy—accurately identifying clinical reactivity. Allergy 60(Suppl. 79):19-26.
- Shaker M, Ventor C. (2016). The ins and outs of managing avoidance diets for allergies. Current Opinion Pediatrics. 28(4):567-572.
- Sicherer SH, Sampson HA. (2010). Food allergy. J Allergy and Clin Immunol 125:S116-125.
- Zhao X, Li L, Kuang Z, Luo G, Li B. (2015). Proteomic and immunological identification of two new allergens from silkworm (Bombyx mori L.) pupae. Central European J Immunology 40(1);30-34.
Please note: This is a commercial profile
© 2019. This work is licensed under CC-BY-NC-ND.