Michelle Vickers, CEO of the Head and Neck Cancer Foundation tells us what we need to know about head and neck cancer treatment, including comment on driving surgical-technological development
At the Head and Neck Cancer Foundation (HNCF), we drive for the awareness and adoption of ground-breaking head and neck cancer treatment. There are over 30 regions in the head and neck where cancer can occur, including the mouth, sinuses and the salivary glands. Traditional head and neck cancer surgery can often have devastating aesthetical impacts such as parts of the face, jaw or tongue being removed. This also leaves patients with difficulties in eating and loss of senses or movement in the face.
At the HNCF, we aim to minimise the magnitude of these surgeries, and the resulting aesthetical impacts on patients, which can seriously impact a patient’s quality of life. Cancer Research UK estimate that there are over 12,000 new cases of head and neck cancer diagnoses each year in the UK alone, equating to 34 new cases a day. They also report that between 19% and 59% of those diagnosed survive their disease for at least ten years. Between 2015 and 2017, there were almost 4,000 deaths attributed to head and neck cancers.
The main priority with head and neck cancers needs to be improving patient outcomes. This is partly done by raising awareness of the cause and explaining the preventative measures people can take against this disease. We need to ensure that patients can maintain as much of their quality of life as possible. For example, at the HNCF, we teach and encourage people to regularly check their mouths for oral lesions and explain the route to follow if they do find abnormalities. This is with the aim to diagnose oral cancers at an earlier stage, as this can increase the chance of survival by up to 90%.
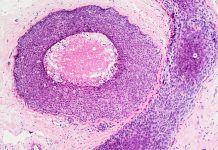
Treatment varies depending on which type of head and neck cancer a patient is diagnosed with. Most surgical treatments are still largely based on invasive techniques. The main priority of head and neck cancer treatment is to remove any cancerous tissue whilst attempting to preserve healthy tissue, minimising any additional damage. Typically, the later cancer is diagnosed in this region, the more extensive the surgery is likely to be. If oral cancers are diagnosed at an advanced stage, extensive measures such as tongue reconstruction with skin grafts may be necessary. Despite the improved prognosis, surgery can often have a massive psychological impact on patients, which may be as equally traumatic as the procedure itself. Patients’ life- saving surgeries may result in them losing the senses of sight, hearing, taste or smell, which can leave them with ongoing trauma and a lower quality of life. Luckily, there is now a range of emerging treatments that are minimally invasive and effective. One example of this is Sentinel Node Biopsy (SNB), pioneered by Professor Mark McGurk and supported by the HNCF. In many cases where a patient has a cancer in a lymph node, SNB can replace the traditional treatment of a full neck dissection, replacing an ear-to-ear operation with one small incision. These new treatments allow for quicker, less invasive surgeries that most importantly greatly reduce the lasting impact of surgery on patients.
Head and neck cancer in deprived areas
For both women and men, the chances of developing head and neck cancer are significantly higher for those living in the most deprived areas of the UK. In England alone, Cancer Research UK estimates that approximately 2,300 cases of head and neck cancer are linked to deprivation and that most of these cases (78%) are in men. Men in the most deprived areas are twice as likely (101%) to get head and neck cancer than those in the least deprived areas. This shows that there is a clear socio-economic issue regarding this specific disease. Although the exact reason is not clear, Professor Sir Michael Marmot of University College London has suggested that this is due to the body’s stress pathways; depriving people of control is a more stressful situation. He states that: “When people are disempowered and feel like they don’t control their lives, why should they bother making healthier choices such as not smoking and eating healthily”. We want to help combat this and show all people that there are preventative measures everybody in society can take.
Surgical-technological development
At the HNCF, we drive surgical-technological development, aiming to further reduce the number of patients with lasting aesthetical impacts. The pioneering research we carry out aims to further improve the outlook for patients, especially those who require surgical intervention, by reducing the aesthetical implications of biopsies, the risk of damage to major facial nerves and preserving the use of all senses. We also put lots of effort into getting as many surgeons and healthcare professionals as possible equipped to use these new techniques. We work to not only save the lives of, but minimise the lasting impact of head and neck cancer on those affected. It all comes down to raising awareness of the disease and making patients aware of the new treatments available to them. The earlier we can diagnose somebody with this specific type of cancer, the more options become available to treat it. A patient’s surgical outcome and quality of life is likely to be better the earlier cancer is caught.
References
https://www.bbc.co.uk/news/health-37923708
https://www.bloomsbury.com/uk/the-health-gap-9781408857991/\