With the number of hip fractures projected to double by 2050, Dr Philippe Halbout, CEO of the International Osteoporosis Foundation, calls for timely action, including post-fracture care to prevent costly and life-threatening secondary fractures
Hip fractures are a major consequence of osteoporosis and are considered the most serious of osteoporosis-related fractures in terms of morbidity and mortality. It is estimated that more than 10 million hip fractures per year occur globally, placing an enormous burden on patients, their families, and healthcare systems.
The great majority of hip fractures occur in seniors aged 65 and older, largely due to the fact that older adults tend to have reduced bone density, muscle strength, and balance. With the rapid ageing of the global population, the number of hip fractures is projected to nearly double by 2050. The increase is expected to be even higher in males due largely to their greater increase in life expectancy.
Stretched healthcare and a lack of support
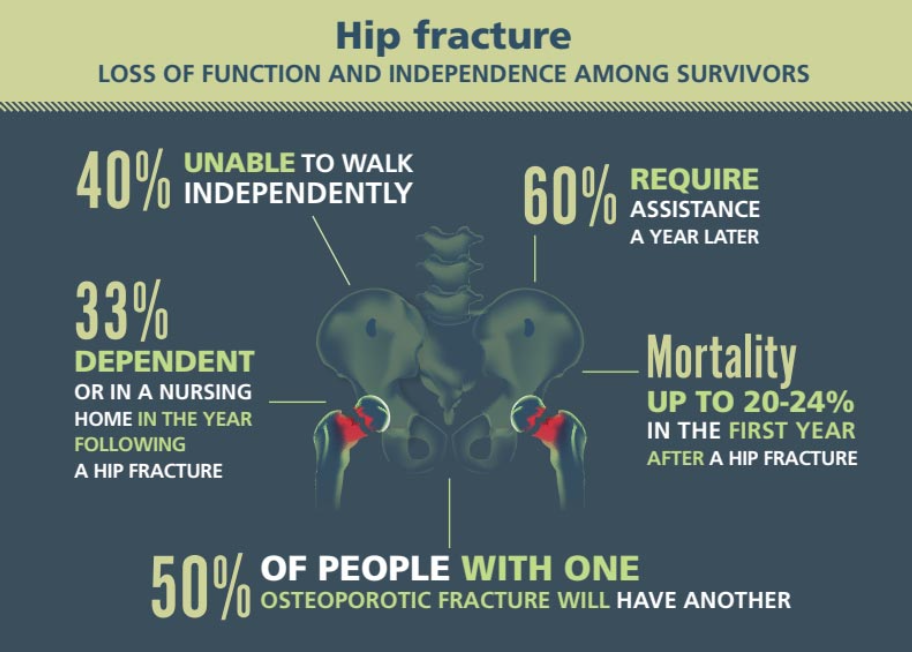
Healthcare systems are now, almost universally, stretched to their limits. The question is: are the world’s healthcare services prepared to cope with this overwhelming increase in hip fractures due to osteoporosis? Hip fractures lead to costly surgeries, hospitalization, need for rehabilitation services, and in many cases, place a heavy burden on family caregivers or result in the need for long-term nursing home care. Mortality is high, with approximately 24% of hip fracture patients dying within the year following their fracture, while survivors often face a profound loss of function and independence. Some 60% of hip fracture patients require assistance a year later, and as many as 33% become totally dependent or enter assisted care homes in the year following the fracture.
The critical issue is that a patient who has suffered a hip fracture is at very high risk of sustaining a further serious and life-threatening fracture in the future, and that risk is highest in the next one to two years. A second hip fracture occurs in approximately one in four patients after any previous osteoporotic fracture and in one in three patients who have sustained a hip fracture, on average, within one and a half years.
Despite the obvious need for timely anti-osteoporosis treatment to prevent secondary fractures, we currently face a tragic situation where the vast majority of people who have experienced a first fracture do not receive anti- osteoporosis medication to help protect against further fractures. This treatment gap reflects the fact that bone health is underprioritized within healthcare systems and by patients and physicians alike worldwide. For example, in the US, only 23% of elderly patients who suffer a hip fracture receive osteoporosis medication to reduce future fracture risk compared to 96% of heart attack patients who receive beta blockers to prevent a future heart attack. This ‘take no action’ approach is inacceptable: we have an array of proven anti- osteoporosis medications at our disposal and medical management guidelines that clearly outline best-practice in diagnosis, treatment and follow-up for osteoporosis and fragility fractures.
Solutions exist: Health authorities need the will to put them into action
So, what can be done to close the treatment gap and reduce the growing burden of hip fractures among the older populations?
To begin with, a change of mindset is needed. All too often, the societal and human costs of fragility fractures are vastly underestimated by policymakers, healthcare professionals and patients alike. We must begin by combatting the myth that osteoporosis is an inevitable process of ageing when, in fact, it is a preventable and treatable disorder.
Through its many educational and public outreach initiatives, the International Osteoporosis Foundation (IOF) seeks to advance a two-pronged approach to fragility fracture prevention. On the one hand, primary prevention must be fostered by raising awareness of bone-healthy lifestyle in the younger population to reduce the risk of osteoporosis in later life. Primary care physicians must also be sensitized to the need for early identification and treatment of at-risk patients in their clinical practices before the first fracture occurs.
The second component of a dual-pronged strategy is the focus on secondary fracture prevention. IOF, in collaboration with national experts worldwide, has identified investment in secondary fracture prevention as a strategic priority, given that it is one of the most efficient ways to stem the rising tide of hip fractures. It’s been likened to ‘grabbing the low-hanging fruit of a tree’: those who are at the highest risk and at the most urgent need of preventative treatment are those who have already broken a bone.
For this reason, IOF has established a successful global programme called Capture the Fracture®. The programme’s mission is to promote the implementation and effectiveness of coordinated post-fracture care services such as Fracture Liaison Services (FLS) in hospitals worldwide. These services, comprising a multidisciplinary team employing a dedicated coordinator to act as the link between the patient and the orthopaedic team, other specialists, falls prevention services, and the primary care physician, work to ensure that fragility fracture patients are evaluated and treated.
Hip fracture patients, for example, are offered appropriate care, including rehabilitation, falls prevention assessment, anti-osteoporosis treatment, and monitoring to help improve outcomes and reduce their high risk of future hip and other osteoporotic fractures. With the widespread implementation of Fracture Liaison Services, we would expect to see notable reductions in the number of recurring fractures.
Evidently, there is much that can and must be done within the broader public, research, medical and policy spheres. The many solutions are clearly outlined in IOF policy publications such as the IOF Compendium of Osteoporosis or the recent Capture the Fracture® Guidance for Policy Shaping.
First and foremost, for real change to happen, health authorities need the determination to allocate resources for the prevention of osteoporosis and fragility fractures. This investment is crucial in safeguarding millions of older adults from the suffering, disability, and loss of independence associated with hip fractures.