The Imaging and Radiation Oncology Core is part of the U.S. National Cancer Institute’s clinical trial program and provides quality assurance for trials with radiation oncology and/or imaging
Unfortunately, medical errors are known to be one of the leading causes of death. Sometimes these errors are glaring mistakes with dramatic and immediate consequences. These provide a clear link between an error and the consequence, and while difficult, this at least allows for the opportunity to understand the error and learn from it, helping prevent similar errors from happening in the future. However, not all situations have such a clear link, and not all situations that can harm the patient are strictly errors. There is a continuum between erroneous care and optimal care, and within this continuum is a large area of suboptimal care; where the practice isn’t where it should be, or at least could be. This suboptimal care may cause problems that manifest later and are less dramatic, making the link between the event and the consequences harder to identify. Nevertheless, such deficiencies may be very serious because they can affect large numbers of patients without being detected.
While the issue of medical quality has received increased attention in recent years, this topic remains understudied and under-resolved. This is in no small part because of the difficulties inherent to studying this topic. The ethical challenges inherent to studying low medical quality are front and centre – how does one allow a patient to receive suboptimal care? But other issues also complicate this question: if the effect of lower quality is a 5% reduction in survival, a large number of patients would be needed in a controlled setting to see this effect. And the quality deficiency would need to be known – if the quality of care is systematically inferior (e.g., a miscalibrated piece of equipment), there may be no readily available baseline to indicate what optimal outcomes should look like. Despite these complications, the issue of quality of care may be at the heart of why outcomes are better or worse at different facilities.
Exploring issues in medical quality
The field of radiation oncology provides an outstanding opportunity to explore the question of medical quality, and through that understanding, improve it and the underlying issues that more broadly affect medical quality. Radiation oncology outcomes are dependent on getting the right dose to the right place. And like any other branch of medicine, it is essential that the correct dose be given to get the desired effect. When patient outcomes have been reviewed in the clinical trial setting, it has been repeatedly shown that patients who received optimal radiotherapy care have much better survival outcomes than those whose treatments have deficiencies. These data show that the risk of suboptimal quality is clearly affecting patients.
Radiation oncology is a uniquely quantitative branch of medicine. When trying to cure disease, it is generally held that the dose must be accurate within 5% to have the desired outcome. Through high precision measurements, it is possible to measure the radiation dose delivered (in a patient surrogate if not in the actual patient) as accurately as within 2%. Given that radiation doses can be measured within 2%, it would be expected that all treatments should fall within the desired 5% accuracy. However, this does not seem to be the case.
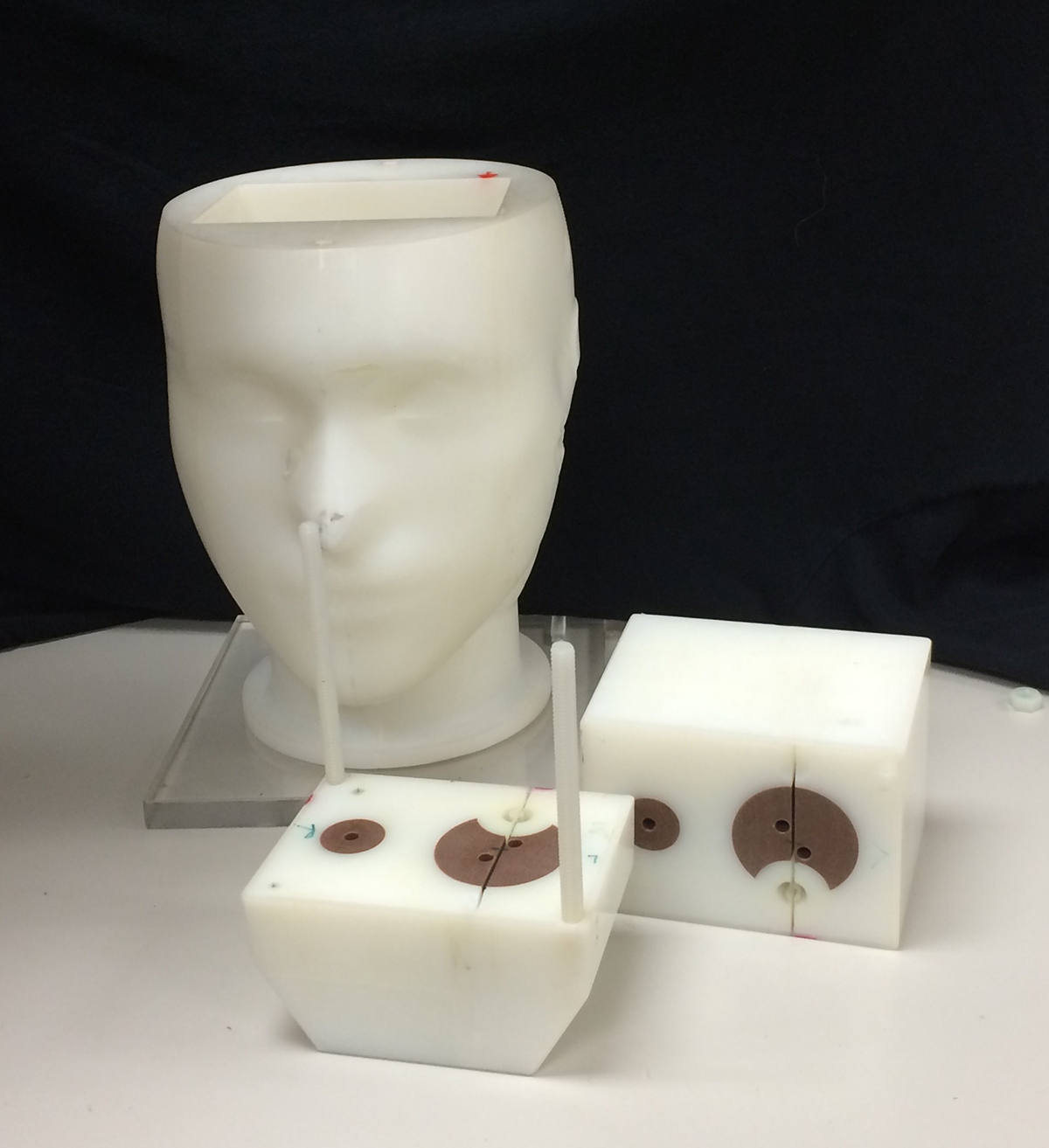
The Imaging and Radiation Oncology Core (IROC) is the largest radiotherapy and imaging quality assurance centre in the world and supports clinical trials from the US’s National Cancer Institute. One tool used by IROC to evaluate the performance capability of institutions wishing to participate in clinical trials is to provide them with a plastic dummy-patient loaded with radiation detectors. This pseudo-patient is mailed to an institution who treats it like a real patient, developing and delivering a treatment. The plastic patient is returned to the Imaging and Radiation Oncology Core and the delivered dose is compared to the intended dose. IROC performs approximately 700 of these plastic patient tests every year at institutions all over the world and has tested several thousand radiotherapy clinics. Unfortunately, while all institutions should be able to deliver the dose within 5%, the result is that more than 30% of institutions fail to do so. In fact, 10-20% of institutions fail to deliver the dose even within 7%.
Large and frequent deficiencies
It is worth noting that the institutions internally evaluate these radiotherapy treatments before delivery. That is, each radiotherapy treatment has been tested and the institution believed they were delivering a highly accurate dose of radiation. It was only upon independent review of their delivery that the deficiency was identified. The fact that such large and frequent deficiencies are observed is not only concerning for the patient but highlights broad problems in radiotherapy dose delivery evaluation.
There are a host of reasons why these errors may be manifesting in current radiotherapy practice. One factor is that technology changes rapidly in radiation oncology to allow for the most conformal radiation dose to be delivered to the tumour. However, this means that new techniques and technology are constantly implemented, introducing an opportunity for suboptimal implementation. Also, while radiation doses can be measured within 2%, many measurement techniques do not achieve this accuracy, highlighting a disconnect between what is expected and what is achieved. This highlights a major and systemic deficiency in the quality of radiotherapy delivery. It is known that lower quality radiotherapy leads to poorer patient outcomes, and a shockingly large percent (up to 30%) of institutions are delivering lower quality than expected and desired. This poses a critical risk to radiotherapy patients that requires more attention to better understand and address.
Reducing medical errors across branches of medicine
More broadly, while there are unique aspects to radiation oncology, it is hard to imagine that these deficiencies don’t also exist in other branches of medicine. The example of radiation oncology should serve as a call to arms of medical practice in general. Addressing isolated major and glaring medical errors is a critical step, but it is not a sufficient step. The quality of the practice of medical care must also be evaluated and maximised. This must include independent peer review, where a subject matter expert can evaluate the quality of the work performance and provide guidance to improve it when appropriate.
Please note: This is a commercial profile
© 2019. This work is licensed under CC-BY-NC-ND.











