With the implementation of the KHPO, knee replacement surgeries would have been unnecessary, sparing patients from significant suffering
Case study:
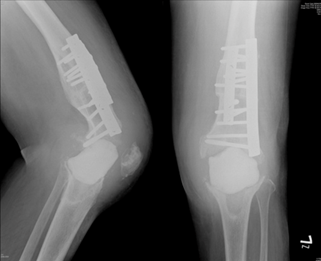
At 7:30 PM one evening, a woman in her fifties was wheeled into my clinic, tears streaming down her face as she pleaded, “Doctor, please help me…” After consoling her patiently, she gradually recounted the past year of suffering, following an unfortunate bacterial infection post total knee replacement surgery. Her left knee, scarred, swollen, and non-functional, along with X-rays provided by her family (see Figure 1), painted a grim picture.
This tragedy brought back a memory from eight years ago, the story of a hardworking seventy-year-old man. Over the span of two agonizing years, he navigated through various hospitals in hopes of finding a solution for the pus-forming infection in his knee after undergoing a knee arthroplasty. Unfortunately, despite multiple surgeries, his wound failed to heal, requiring frequent medication changes to alleviate the pain. With a desire for recovery, the elderly man sought help far and wide.
Yet, his condition was far more severe than anticipated, not amenable to a simple arthroscopic washing procedure. I explained to him in detail the two-stage surgical procedure that needed to be implemented. Firstly, removal of the infected artificial joint and implantation of antibiotic-laden material, followed by the installation of a new artificial joint after complete eradication of the bacteria three months later. Due to previous failed attempts with similar treatments, the elderly man found it challenging to accept this proposal and eventually chose to depart.
Tragically, three days later, news relayed by his neighbor through a phone call reached us – the elderly man had chosen to end his own life. The news hit me like a sledgehammer, with thoughts of the old man’s suffering in his later years filling my heart with endless sorrow and reflection. His story serves as a reminder that each treatment decision requires careful consideration. More importantly, we need to listen patiently to patients, understanding their fears and hopes.
In the medical field, we are not just healers of the body but also soothers of the soul; our mission is to extend a helping hand to patients when they need it most, offering hope and courage, showing them that no matter how challenging the road ahead may be, a ray of light is always waiting for them. These experiences remind me how crucial it is to approach artificial joint replacement with extreme caution.
Now, let’s go back to the current patient.
I decided that the priority was to calm her emotions. Then, based on her specific circumstances, we discussed treatment plans. Upon detailed inquiry, we discovered that the post-operative treatment she received after the removal of the artificial joint was inadequate – insufficient antibiotic use and improper knee stabilization. Consequently, we devised a first-stage treatment plan for her: no surgery immediately, but hospitalization for a six-week course of antibiotic treatment and muscle rehab to alleviate inflammation and rebuild confidence, followed by a consideration for surgical treatment. Bacterial infections have posed significant challenges in the medical field. Even in operating rooms equipped with the most advanced equipment, the risk of infection persists at a rate of 0.3% to 5%.
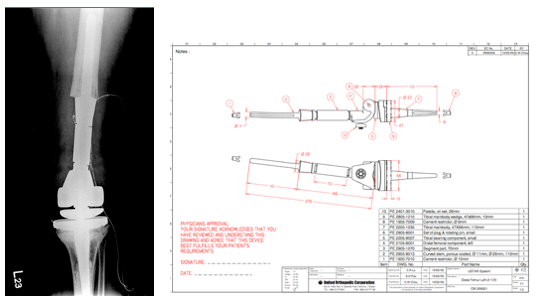
In contrast, traditional older-style operating rooms lacking laminar airflow facilities see a substantial increase in infection rates to 3% to 5%. The management and treatment process post-infection are prolonged and arduous, posing a significant challenge to both patients and healthcare workers. Considering the patient’s unique situation, we meticulously planned a suitable surgical approach. Given the severe bone damage near her knee, rendering common artificial joint models unsuitable, we worked closely with engineers to custom design a long-stem artificial joint (see Figure 2).
Through this case, we witness the profound impact of medical expertise on a patient’s quality of life, underscoring the importance for patients and physicians to fully understand the risks and consequences when choosing treatment plans. Each surgery is not just a display of technical skill but also a testament to the reverence and responsibility we hold for life. I hope this story encourages deeper reflection on medical decision-making and offers hope to those facing similar challenges.
Why were those knee replacement surgeries unnecessary and avoidable?
I have researched and documented, through our published journal articles1-16, that:
- Knee osteoarthritis (OA) is not simply the result of degeneration or aging.
- The presence of fibrotic medial plica in the knee capsule contributes to medial abrasion phenomenon (MAP), which can lead to OA.
- The Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP) effectively eliminates the medial abrasion phenomenon (MAP) and relieves pressure on the patellofemoral joints, helping to reduce knee pain and potentially reverse the progression of knee OA in patients.
- If traditional knee replacement surgery fails to address the MAP, patients may continue to experience pain or discomfort.
In our practice, we have successfully performed ACRFP—a minimally invasive arthroscopic procedure—over 10,000 times during the past 20 years. Our patients have found relief from knee pain while retaining their natural knees. Because our ACRFP patients did not undergo knee replacement surgeries, they avoided the risk of infections that two patients—treated by different physicians—suffered.
If those two patients had sought treatment by KHPO, they might not have experienced such complications. Their infections arose from knee replacement surgeries, which we would have replaced with the ACRFP under KHPO, a method we have proven to make knee replacements avoidable if performed in time.
References
- Lyu S-R, Hsu C-C, Hung J-P, Chou L-C. Arthroscopic cartilage regeneration facilitating procedure can modify the clinical course of knee osteoarthritis. Journal of Orthopaedic Surgery. 2023;31(2). doi:10.1177/10225536231180331.
- Lyu SR, Hsu CC, Hung JP, Chou LC, Chen YR, Lin CW. Arthroscopic cartilage regeneration facilitating procedure: A decompressing arthroplasty for knee osteoarthritis. Medicine (Baltimore). 2022 Sep 30;101(39):e30895. doi: 10.1097/MD.0000000000030895. PMID: 36181017; PMCID: PMC9524980.
- Lyu S-R, Hsu C-C, Hung J-P. Medial abrasion syndrome: a neglected cause of persistent pain after knee arthroplasty. J Orthop Surg Res. 2021;16(1).
- Tsung-Chiao Wu, Chuan-Hsin Yen, Shaw-Ruey Lyu, Shuo-Suei Hung. Modification in foot pressure and gait pattern after arthroscopic cartilage regeneration pacilitating procedure (ACRFP)l in patients with osteoarthritis of knee. Journal of Mechanics in Medicine and Biology Vol. 19, No. 2 (2019) 1940026.
- R. Lyu, Knee health promotion option for knee osteoarthritis: a preliminary report of a concept of multidisciplinary management, Healthy Ageing Research, 4-34, 2015.
- R. Lyu, D.S. Liu, C.E. Tseng, H.S. Wang and L.K. Chau, Role of medial abrasion phenomenon in the pathogenesis of knee osteoarthritis, Medical Hypotheses, 85(2), 207-211, 2015.
- Shaw-Ruey Lyu, Ching-Chih Lee, Chia-Chen Hsu, Medial abrasion syndrome: a neglected cause of knee pain in middle and old age, Medicine, 94(16), e736, 2015.
- S. Liu, Z.W. Zhuang, S.R. Lyu. Relationship between medial plica and medial femoral condyle—a three-dimensional dynamic finite element model. Clinical Biomechanics. Volume 28, Issues 9–10, November–December 2013, Pages 1000–1005.
- Chih-Chang Yang, Cheng-Yu Lin, Hwai-Shi Wang, Shaw-Ruey Lyu, Matrix Metalloproteases and Tissue Inhibitors of Metalloproteinases in Medial Plica and Pannus-like Tissue Contribute to Knee Osteoarthritis Progression. PLoS ONE 8(11): e79662. doi:10.1371/journal.pone.0079662.
- Shaw-Ruey Lyu, Chia-Chen Hsu and Chih-Wen Lin, Arthroscopic cartilage regeneration facilitating procedure for osteoarthritic knee. BMC Musculoskeletal Disorders 2012, 13:226, http://www.biomedcentral.com/1471-2474/13/226.
- Wang, H. S., Kuo, P. Y., Yang, C. C., & Lyu, S. R. (2011). Matrix metalloprotease-3 expression in medial plica and pannus-like tissue in knees from patients with medial compartment osteoarthritis. Histopathology, 2011, 58(4), 593-600.
- Lyu SR, Chiang JK, and Tseng CE, Medial plica in patients with knee osteoarthritis: a histomorphological study, Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA, 2010,18(6):769-76.
- Shaw-Ruey Lyu, Arthroscopic medial release for medial compartment osteoarthritis of the knee, J Bone Joint Surg Br, September, 2008, Vol 90-B, issue 9, Pages 1186-1192.
- Shaw-Ruey Lyu, Relationship of medial plica and medial femoral condyle during flexion. Clinical Biomechanics, 2007, Volume 22, Issue 9, Pages 1013-1016.
- Shaw-Ruey Lyu, Jeh-En Tzeng, Chia-Yuan Kuo, Ai-Ru Jian, De-Shin Liu Mechanical strength of mediopatellar plica-The influence of its fiber content Clinical Biomechanics, Volume 21, Issue 8, October 2006, Pages 860-863.
- Lyu SR, Hsu CC, Medial plicae and degeneration of the medial femoral condyle. Arthroscopy. 2006 Jan;22(1):17-26.