Michelle Davis, Head of External Relations at Malaria Consortium, shares with us what we need to know about learning from COVID-19 and the continuing fight against malaria
In countries where the disease burden of malaria is high, health systems have long felt the strain as governments seek to reduce its devastating impact. The positive news is that we are now at a tipping point in many countries where we know malaria can be beaten, even in remote communities, and areas affected by protracted conflict. Huge gains have been made since the Abuja Declaration of 2000 but those gains are fragile, with the pandemic serving only to exacerbate.
Malaria burden reduction is still possible with the right tools, investment & infrastructure
Reducing the burden of malaria is possible when: the appropriate tools are available for prevention and accurate and timely diagnosis and treatment, the latter increasingly being supported with digital solutions; when domestic and other funding are prioritised and there is long-term and meaningful community engagement to improve demand for and sustainability of health services; and when there is robust disease surveillance and response infrastructure capable of identifying outbreaks, alongside a culture of data-informed decision-making.
Disease surveillance and response must identify outliers/outbreaks of diseases otherwise in control
In the 16 months since COVID-19 was declared a global pandemic, countries have focused on containment and recovery, with an understandable need to re-allocate resources – both human and financial – to manage disease outbreaks. However, with a focus on malaria burden reduction – effective surveillance, differential diagnosis and response remain critical, with an additional priority of building community resilience to outbreaks as we move towards elimination. Surveillance and response approaches need to be carefully considered, resourced and planned.
Digital solutions at community level strengthen disease control
The COVID-19 pandemic has highlighted the potential of digital solutions to improve prevention, diagnosis and treatment of disease. In Mozambique, support was given for community health workers, who play a critical role in managing infectious diseases, to respond to the pandemic. By making adaptations made to the country’s existing upSCALE digital platform, COVID-19 health messages were provided for the community health workers. With misinformation arising from a lack of accurate and up-to-date evidence on the virus, supporting the accurate diagnosis of the disease at the community level is critical in helping to reduce the burden not only of COVID-19, but also of diseases such as malaria and pneumonia, which have similar symptoms.
Major interventions were still possible despite COVID-19
2020 presented new challenges for implementing community-based malaria control interventions. This included seasonal malaria chemoprevention (SMC), one of the most effective, preventive interventions for children aged five and under in areas where transmission is highly seasonal. Our 2020 campaign reached more than 12 million children and was implemented while following strict infection prevention and control (IPC) measures to minimise the risk of transmitting COVID-19. The measures were central to the safe implementation of the campaign, and their adoption into national guidelines to inform the 2021 campaign remains essential. SMC campaigns also proved a powerful platform to share vital other public health information on COVID-19 prevention and transmission.
Community engagement critical to eliminate malaria & COVID-19
In many countries, with community engagement, life- saving interventions have continued to be delivered. In South Sudan, long-lasting insecticidal nets (LLINs) are among the most widespread and cost-effective prevention methods used to combat malaria. While COVID-19 threatened to disrupt LLIN distribution, amplifying community engagement ensured community-led activities helped address challenges around net distribution, overlaid with social and behaviour change approaches to help address deep-rooted, health-related behaviours that were limiting the adoption of COVID-19 transmission-prevention guidelines. Observing respected individuals engaging in preventive practices ultimately encouraged communities to adopt similar behaviours.
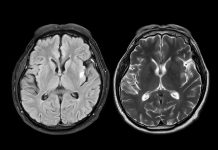
Understand comorbidities to make a difference to a health system
The potential implications of clinical interactions between COVID-19 and malaria – and any other disease – is a major public health concern in Africa. In 2020, together with the Ugandan Ministry of Health, we undertook research to better characterise COVID-19 cases in a high malaria burden setting and to determine the prevalence and describe the clinical consequences of SARS-CoV-2 and malaria co-infection. Our preliminary findings, recently published in preprint in The Lancet, show that high exposure to malaria appears to reduce the risk of severity of COVID-19. More research is needed to better understand the relationship between the two diseases, but these early findings (awaiting peer review) are significant and may help us to understand why the impact of COVID-19 in Africa has not been as severe as initially anticipated.
Globally, even the most resilient and best-equipped health systems are struggling to recover from COVID-19- related shocks. It is, therefore, more important than ever to remain vigilant to the serious public health threat that malaria continues to pose, as we work towards controlling and eventually eliminating the disease.
Vector-borne diseases spotlight
Vector-borne diseases cause over 700,000 deaths each year and account for at least 17% of all infectious diseases. Vector-borne diseases are caused by either bacteria, parasites or viruses. “Vectors are living organisms that can transmit infectious pathogens between humans, or from animals to humans,” according to the WHO.
In addition, the burden of vector-borne diseases are the highest in tropical and subtropical areas and disproportionately impact the poorest populations. The WHO goes on to explain that “Since 2014, major outbreaks of dengue, malaria, chikungunya, yellow fever and Zika have afflicted populations, claimed lives, and overwhelmed health systems in many countries.” (1)
When we look at the Division of Vector-Borne Diseases (DVDB), within the U.S. CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), we see that they aim, “to create a future where vector-borne diseases no longer threaten public health”. This is certainly a challenge considering the aforementioned discussion concerning the extent of vector-borne diseases globally today.
• To reduce death and illness from vector-borne diseases, the DVDB has four goals, which are:
• To detect and identify and vector-borne pathogens that cause diseases in human beings.
• To find out when, where, how often plus how individuals are vulnerable to vector-borne pathogens.
• To mitigate the consequences of infection and prevent exposure to vector-borne pathogens.
• To set up disease diagnostics, surveillance, control and prevention programmes. (2)
Considering the wider picture, we know that vector-borne diseases are a priority as part of the CDC’s strategy to secure global health and America’s preparedness to address diseases threats. (3) Looking ahead, one way to advance discovery and innovation is by research and development by universities, industry and government, “to develop ways to foster new vector control technologies and monitor and prevent insecticide resistance.” (4)
References
1. https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases
2. https://www.cdc.gov/ncezid/dvbd/about.html
3. https://www.cdc.gov/about/organization/strategic-framework/index.html
4. https://www.cdc.gov/ncezid/dvbd/about/prepare-nation.html