Abbas Kanani, Superintendent Pharmacist at Chemist Click Online Pharmacy, walks us through what we need to know about living with diabetes, starting with a comment on prediabetes
Prediabetes is when blood sugar levels are higher than usual but not yet high enough to be classified as type 2 diabetes. Prediabetes is a warning sign that a person’s blood sugar levels are becoming elevated and that they are at increased risk of developing type 2 diabetes and other related health problems, such as heart disease and stroke.
Defining type 1 & type 2 diabetes?
Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks and destroys the cells in the pancreas that produce insulin. As a result, patients cannot produce insulin and must take insulin injections or use an insulin pump to manage their blood sugar levels. Type 1 diabetes is typically diagnosed in children and young adults and is considered a lifelong condition.
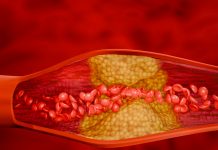
Type 2 diabetes is the most common form of diabetes and is caused by a combination of genetics and lifestyle factors, such as being overweight, having a sedentary lifestyle, and following an unhealthy diet. In type 2 diabetes, the body becomes resistant to the effects of insulin, and the pancreas gradually loses its ability to produce enough insulin to regulate blood sugar levels.
People with type 2 diabetes may initially be able to manage their condition through lifestyle changes, such as healthier eating and increased physical activity. Still, many living with diabetes eventually require medication, such as oral drugs or insulin injections, to manage their blood sugar levels.
How scientists across are pushing boundaries with diabetes research Researchers have developed artificial pancreas systems that use continuous glucose monitoring and insulin pumps to automate the delivery of insulin and regulate blood sugar levels in real-time, with the potential to improve the lives of people with diabetes significantly.
Pancreatic islets produce insulin, allowing us to regulate blood sugar levels. In addition, it is possible to have a transplant from a donated pancreas, allowing type 1 diabetics to produce their own insulin.
Researchers are also working on developing non-invasive glucose monitoring technologies for people living with diabetes, such as wearable devices and implantable sensors, that can accurately measure blood sugar levels without the need for finger sticks, making monitoring more convenient and less painful.
New and innovative ways to improve insulin therapy are also being explored, such as developing new formulations of insulin that work faster, last longer, and are less prone to causing low blood sugar.

Treatments to help manage & treat diabetes
When living with diabetes, we need to understand there is no cure, but people can lead healthy, active lives with proper treatment and management. The specific treatment plan for an individual living with diabetes will depend on various factors, including the type of diabetes they have, overall health, and lifestyle. Therefore, it should be tailored to their specific needs, which may change over time as their condition and health status change.
Lifestyle changes such as healthy eating, regular physical activity, and weight management can help improve blood sugar control and reduce the risk of complications for people with type 2 diabetes.
Oral medications such as metformin, sulfonylureas, meglitinides, and DPP-4 inhibitors also help to lower blood sugar levels and improve insulin sensitivity. In addition, bariatric surgery such as gastric bypass or sleeve gastrectomy may be recommended to help severely overweight type 2 diabetics lose weight and improve blood sugar control.
For people with type 1 diabetes or advanced type 2 diabetes, insulin therapy may be necessary to regulate blood sugar levels. Continuous glucose monitoring (CGM) and insulin pump therapy can also help people with type 1 diabetes automate insulin delivery and regulate blood sugar levels in real time.
Discoveries transforming diabetes care
The discovery of insulin by Canadian scientists Frederick Banting and Charles Best in 1921 was a significant turning point in treating diabetes. Before this discovery, people with diabetes often did not live very long. With insulin therapy, people can regulate their blood sugar levels and extend their lifespan.
The development of continuous glucose monitoring (CGM) technology has revolutionized diabetes care by allowing patients to continuously monitor their blood sugar levels in real time, avoiding dangerous highs and lows.
Insulin pump technology allows patients to receive insulin in a continuous, controlled manner, which helps to improve blood sugar control and reduce the risk of complications advances in insulin therapy, such as the development of rapid-acting insulin analogues and long-acting insulin formulations, have improved the convenience and effectiveness of therapy.
Bariatric surgery has emerged as a promising treatment option for people with type 2 diabetes who are severely overweight. Aiding weight loss and improving insulin sensitivity, bariatric surgery can significantly impact blood sugar control and overall health.
Lastly, the development of telehealth has allowed patients to receive care and support from their healthcare providers remotely. They can receive diabetes education, adjust medications, and monitor blood sugar levels, all from the comfort of their homes.
Funding diabetes research
In the UK, Europe, and other regions, funding for diabetes research has contributed to major advancements in the field, including the development of new medications, insulin therapies, and medical devices, as well as a deeper understanding of the underlying causes of diabetes.
By investing in diabetes research, we can improve the diagnosis, treatment, and management of diabetes and reduce the disease burden on individuals, families, and society as a whole. Funding for diabetes research can also drive innovation, create new opportunities for economic growth and job creation, and help attract top talent to the field.