Zisis Kozlakidis from the World Health Organization’s International Agency for Cancer and Jiaao Yu from the Shanghai Jiao Tong University discuss the burden of lung cancer in Southeast Asia and China and the priorities for therapies and interventions
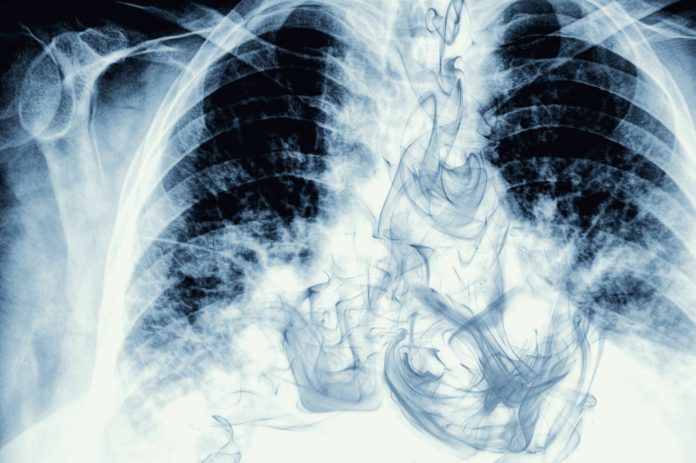
Lung cancer remains a significant public health concern globally and also regionally in Southeast Asia and China, accounting for a substantial burden of disease. According to the IARC, it is estimated that there were 1.2 million new cases in Southeast Asia and China in 2022. Despite the advancements in diagnosis and treatment, significant challenges persist. This article assesses the current state of knowledge regarding lung cancer in Southeast Asia and China, identifies key research gaps, and proposes priorities for future research and intervention.
Smoking and lung cancer in Southeast Asia and China
Lung cancer ranks as the first and second leading
cause of cancer-related deaths for men and women, respectively, in Southeast Asia, while standing as the primary cause of cancer-related deaths for both genders in China. The policies have embraced a multi-pronged approach, including primary objectives: the understanding of tobacco consumption within regional contexts; the prevention of smoking by targeted measures (addressing starting, as well as cessation initiatives); the increase of diagnosis for cancer; the increase in taxation; and the availability of new treatments for lung cancer where possible. Although persistent efforts have been made to control tobacco consumption, cigarette smoking remains the primary risk factor for lung cancer in these countries.
The prevalence of tobacco smoking is 43.7% and 47.6% among male adults in Southeast Asia and China, respectively, contributing to individual exposure but also to significant exposure to second-hand smoke for the general population. (1)
For screening for lung cancer in individuals aged 50 to 80 with a 20-pack-year smoking history or more within a clinical setting, the American Cancer Society recommends a low-dose CT scan. In China, such chest CT scans have been widely adopted as a screening tool for high-risk populations, resulting in the increasing detection of more early-stage lung cancer cases. However, many Southeast Asian countries lack the necessary facilities and policies to promote large-scale lung cancer screening. Limited availability and the high cost of CT scans in remote areas continue to contribute to delayed diagnoses of lung cancer, leading to advanced disease stages and poor survival rates. There exists a pressing need for higher investment in the equipment and infrastructure necessary to support the expansion of public lung cancer screening programs.
Research gaps
Despite significant efforts in lung cancer screening among smokers, the incidence of lung cancer in non-smoking populations should not be overlooked. A correlation between severe air pollution and the occurrence of lung adenocarcinoma in non-smokers has been found. (2) In addition, Southeast Asia is among the highest polluted regions, with an increasing number of non-smoking lung cancer patients. However, the mechanism by which the pollutants contribute to the carcinogenesis of lung cancer remains unclear. (3) Thus, the impact of air pollution on lung cancer incidence and the need for lung cancer screening in the non-smoking population warrants further investigation.
The use of smokeless tobacco products, including chewing tobacco, water pipes, and vaping, presents an additional significant health concern, particularly in Southeast Asia. Recent studies have revealed an elevated risk of lung cancer among smokeless tobacco users, highlighting the need for public awareness and tobacco control measures. In light of the increasing prevalence of smokeless tobacco use in this region, further investigation should be engaged to elucidate the precise correlation between smokeless tobacco consumption and the incidence of lung cancer.
However, these research areas require expertise that will lead to the identification and promotion of the study of relevant cases. The current levels of available expertise, though, remain very low throughout the region. For instance, in Indonesia, there are only 1500 pulmonologists serving a population of over 270 million people, (4) indicating an urgent need for training practitioners in relevant medical specialties.
Priorities for therapies and interventions
With the emergence of new drugs, treatment options, such as targeted therapy aimed at genetic mutations and immunotherapy, which inhibits immune-system checkpoints, have gradually become the frontline therapy for non-small-cell lung cancer (NSCLC), which is more resistant to chemotherapy. China and some Southeast Asian countries like Thailand, Vietnam, and Malaysia have set up standardized processes of first-line NSCLC treatments based on the targetable mutations such as EGFR, ALK, and ROS1. However, biomarker testing for mutations remains limited across most Southeast Asian countries. Drug availability is another concern of immunotherapy. The approvals of new drugs in most Southeast Asian countries and China are postponed, resulting in a lag in immunotherapy-related treatments. Besides, some of the drugs are not covered by national medical insurance. Furthermore, the discrepancies in genetic susceptibility among different ethnic groups should also be considered. For example, Chinese lung cancer patients tend to have a higher rate of EGFR mutation and lower KRAS mutation compared to European and American populations, (5) underscoring the need for establishing national guidelines for systematic lung cancer treatment based on population genetics.
Despite ongoing advancements in lung cancer prevention, screening, and treatment, lung cancer persists as a leading cause of mortality in Southeast Asia and China. New forms of tobacco consumption, second-hand smoke as well as environmental pollution have been added as contributing factors in our understanding of lung cancer development. Yet, they constitute a greater challenge for its prevention. Collaborations in lung cancer research and regional guidelines among these nations are expected. Additionally, more resources should be allocated to support ongoing research and to address the significant overall burden of lung cancer in Southeast Asia and China.
Where authors are identified as personnel of the International Agency for Research on Cancer/WHO, the authors alone are responsible for the views expressed in this article. They do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer/WHO.
References
- Leiter A, Veluswamy RR, Wisnivesky JP. The global burden of lung cancer: current status and future trends. Nature Reviews Clinical Oncology. 2023;20(9):624-39.
- Hill W, Lim EL, Weeden CE, Lee C, Augustine M, Chen K, et al. Lung adenocarcinoma promotion by air pollutants. Nature. 2023;616(7955):159-67.
- Berg CD, Schiller JH, Boffetta P, Cai J, Connolly C, Kerpel-Fronius A, et al. Air Pollution and Lung Cancer: A Review by International Association for the Study of Lung Cancer Early Detection and Screening Committee. Journal of Thoracic Oncology. 2023;18(10):1277-89.
- Rajadurai P, How SH, Liam CK, Sachithanandan A, Soon SY, Tho LM. Lung Cancer in Malaysia. Journal of Thoracic Oncology. 2020;15(3):317-23.
- Peng W, Li B, Li J, Chang L, Bai J, Yi Y, et al. Clinical and genomic features of Chinese lung cancer patients with germline mutations. Nat Commun. 2022;13(1):1268.