The Medicines and Healthcare products Regulatory Agency (MHRA) has approved the first treatment for Alzheimer’s in Great Britain that shows evidence of slowing progression of the disease; however, it is not recommended for use on the NHS
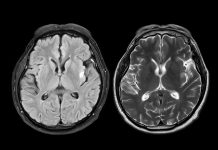
Lecanemab is a monoclonal antibody which binds to a protein called amyloid beta. In Alzheimer’s disease, clumps of amyloid beta protein form plaques in the brain. Lecanemab works by binding to these clumps and reducing them, therefore slowing the progression of the disease.
During trials, lecanemab demonstrated a statistically significant reduction in clinical decline after 18 months.
Lecanemab has been approved to treat adults in the early stages of Alzheimer’s disease who have one or no copies of the apolipoprotein E4 gene (ApoE4).
A 10mg/kg dose is administered intravenously every two weeks under the supervision of a healthcare professional, with each infusion lasting approximately one hour.
Appropriate regulatory standards Lecanemab have been met
Julian Beach, MHRA Interim Executive Director, Healthcare Quality and Access, said: “Licensing medicines which meet acceptable standards of safety, quality and efficacy is a key priority for us.
“We’re assured that, together with the conditions of the licence approval, the appropriate regulatory standards for this medicine have been met.
“As with all medical products, we will keep its safety under close review, and with a controlled post-authorisation safety study to be undertaken, we will ensure that the benefit risk of lecanemab in clinical use is closely followed up.”
The most common side effects are infusion-related reactions (which can cause fever and flu-like symptoms), headaches and Amyloid Related Imaging Abnormalities (ARIAs).
Too expensive for the NHS
However, NICE said in its draft guidance that the benefits of the new Alzheimer’s drug lecanemab are too small to justify the costs, and there is a lack of evidence on its long-term effects. Therefore, it is not recommended for use on the NHS.
Dr Samantha Roberts, chief executive of NICE, said: “This is a new and emerging field of medicine which will no doubt develop rapidly. However, the reality is that the benefits this first treatment provides are just too small to justify the significant cost to the NHS.
“It is an intensive treatment to give to patients involving a hospital visit every two weeks with skilled staff needed to monitor them for signs of serious side effects, plus the cost of purchasing the drug.
“Our independent committee has rigorously evaluated the available evidence, including the benefit for carers but NICE must only recommend treatments that offer good value to the taxpayer.”