Dr Zisis Kozlakidis directs our thoughts towards the molecular aspects of global Infection Prevention and Control, in this the second of a special two-part series
Infection Prevention and Control (IPC) is a practical, evidence-based approach that prevents patients and health workers from being harmed by avoidable infections. IPC informs the practices for hospital environments and forms the basis for many health policies for the wider public.
The technological advances of the last decade have placed the molecular aspects within the core of IPC and also of infections in non-hospital settings, as it is becoming increasingly possible to identify the species of the pathogen(s) causing the infection, but also based on their genomic information to further identify the different types of the organisms within the species. The choice of an appropriate molecular typing method (or methods) depends significantly on the question asked and the epidemiological context in which the method is going to be used, as well as the time and location of acquiring the sample tested.
Importantly, human pathogens of one species can comprise very diverse organisms, and within those organisms, some have additional characteristics such as multiple drug resistance. Therefore, typing techniques should have excellent ‘typeability’ to be able to type all the isolates studied.(1) Here, we consider some of the key molecular aspects of Infection Prevention and Control as they have emerged in the last decade.
Molecular investigation of outbreaks
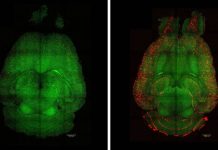
In infectious disease outbreak investigations, a typing method must have the discriminatory power to distinguish between all epidemiologically related and unrelated samples, i.e., those that are part of the outbreak, against a background of circulating infections. In the best-case scenario, such a method should be able to reveal person-to-person transmissions, which is important to develop strategies to prevent further spread. However, the latter is technically still difficult to achieve.
For example, in the recent COVID-19 pandemic, where molecular typing methods were implemented widely,(2) clusters/groups of infections by the same variant virus could be identified; however, the discrimination power could not consistently support the detection of person-to-person transmissions. Having said that, the molecular investigations, combined with epidemiological data, were crucial throughout the pandemic in supporting the implementation of successful Infection Prevention and Control policies globally.
Infectious disease outbreaks require the ability for public health responses to scale up and/or down their responses rapidly
The challenge of molecular investigation of outbreaks is that the methods used must confer at the same time a number of characteristics: they must be rapid, inexpensive, highly reproducible, and easy to perform and interpret. The inexpensive aspect relates directly to the needed deployment in resource-restricted settings where most such outbreaks occur, while the reproducibility and ease of interpretation directly relate to the need for scalability, as infectious disease outbreaks often require the ability for public health responses to scale up and/or down their responses rapidly.
Finally, the data should be sufficiently ‘portable’ and of high quality so that they can be transferable between different systems and be used by international networks. The Global Antimicrobial Resistance and Use Surveillance System (GLASS) launched by the World Health Organization in 2015 is the first global collaborative effort to standardise AMR surveillance and provides the blueprint for the expansion of such approaches to other infectious disease surveillance as part of a global IPC.(3)
Understanding molecular mechanisms and AMR
One of the main reasons why Infection Prevention and Control is quickly becoming a requirement for healthcare is the emergence of anti-microbial resistance (AMR). Bacterial AMR- which occurs when changes in the genetic information of the bacteria cause the drugs used to treat infections to become less effective- is one of the leading public health threats of the 21st century. The detailed molecular characterisation of infectious agents, beyond the benefits mentioned previously, allows for a better understanding of the molecular mechanisms that give rise to AMR. The intensive research of the various molecular mechanisms of AMR has revealed scores of antibiotic resistance genes, or bacterial genes, where certain variants are strongly associated with antibiotic resistance.
This also indicates that there are many (and often overlapping) mechanisms by which AMR can emerge in pathogen populations. In supporting the standardization and sharing of such information, the U.S. National Institutes of Health have developed the National Database of Antibiotic Resistant Organisms (NDARO), a collaborative, cross-agency, centralized hub for researchers to access AMR data, and to facilitate real-time surveillance of pathogenic organisms.(4) The advent of whole genome sequencing (WGS), i.e., decoding the entirety of the genomic information for an organism; permitting quick access to the pathogen genomes; and the collection of sufficiently large datasets of clinical isolates, will all allow to employ of advanced bioinformatics approaches to gain new insights in the more complex molecular mechanisms of AMR.
Technological innovations and Infection Prevention and Control
Conclusively, it becomes evident that while significant technological strides have been achieved in IPC through the inclusion of molecular approaches, the information generated routinely, in particular genetic information, still holds promise for further advances. For instance, being able to understand the more complex mechanisms of AMR emergence is likely to also afford us the opportunity to design more effective antimicrobials or entirely new families of antimicrobials.
Having said that, significant challenges remain, such as the deployment of molecular surveillance capacities in resource-restricted settings, where they are needed most, and the ability to standardize the share the collected information routinely so that the necessary critical mass of knowledge is able to be both impactful and available globally.
References
1. Struelens MJ. Consensus guidelines for appropriate use and evaluation of microbial epidemiologic typing systems. Clin Microbiol Infect. 1996;2(1):2-11.
2. Vandenberg, Olivier, et al. “Considerations for diagnostic COVID-19 tests.” Nature Reviews Microbiology 19.3 (2021): 171-183.
3. World Health Organization (WHO). Global Antimicrobial Resistance and Use Surveillance System (GLASS). Available at: https://www.who.int/initiatives/glass
4. National Institutes of Health. NCBI National Database of Antibiotic Resistant Organisms (NDARO), U.S. Available at: https://www.ncbi.nlm.nih.gov/pathogens/antimicrobial-resistance/
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer/WHO, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/WHO.