Charles H. Vite, DVM, PhD from School of Veterinary Medicine at University of Pennsylvania, focuses on a fascinating aspect of neurological disorders concerning developing therapies for cats, dogs & patients
For many debilitating genetic neurological disorders, there are no satisfactory therapies. For rare diseases, even the natural history of the disease may not be well-understood due to the small number of patients. To understand disease progression and develop effective and safe therapies for diseases of the nervous system, naturally occurring hereditary diseases in cats and dogs are useful models. Working together, veterinarians, physicians and researchers are poised to develop therapies for diseases that have escaped cures in the past (1,2).
The development of effective therapies for many debilitating neurogenetic disorders in patients is limited by 1) the relatively low incidence and high heterogeneity of these diseases, 2) an insufficient understanding of how the genetic defect results in the phenotypic abnormalities, 3) the paucity of validated surrogate markers that can be monitored as secondary clinical endpoints, and 4) the dearth of available and potential therapies which substantially improve disease in animal models.
Small and large animal models
Murine models have been critical to the development of successful therapies. The ability to study both naturally occurring and engineered diseases in mouse models has led to the development of many therapies over the past 50 years which have positively influenced patient care. However, mouse models have limitations due to low genetic diversity, and due to their small size and short lifespan.
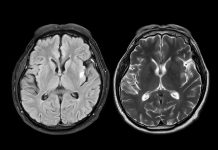
Large animal models serve as important intermediates for the assessment of therapeutic strategies by allowing for 1) natural history studies using large groups of animals with identical disease-causing mutations on a genetic background more varied than that found in inbred rodents but less varied than found in human patients; 2) evaluation of disease progression and safety of therapy using the same equipment (MRI, CT, PET, electrodiagnostic equipment) used in pediatric and general human patient populations; 3) repeated sampling of fluids and tissue; 4) accurate biodistribution studies due to increased brain and body size; and 5) long-term efficacy and safety studies due to their prolonged lifespan. Although non-human primates, sheep and pig models share some of these attributes, naturally occurring diseases are rarely identified in non-human primates, and the vast behavioural, clinicopathological, physiological, and anatomical knowledge available regarding dogs and cats far surpasses what is available in ovine and porcine species.
Disease phenotyping
Characterising neurological disease is performed through the tremendous expertise of international veterinarians (frequently specialised veterinary neurologists) and state-of-the-art veterinary facilities. Examinations available in many specialised veterinary clinics include both routine and specialised physical, laboratory, radiological, ultrasound, magnetic resonance and electrodiagnostic diagnostic procedures. Indeed, in addition to Neurology, areas of veterinary specialisation include Anaesthesia, Behaviour, Ophthalmology, Paediatrics, Genetics, Reproduction, Endocrinology, Cardiology, Dermatology, Internal Medicine, Pathology, Nephrology, Oncology, Haematology, Radiology, Clinical Pathology, Immunology, Nutrition and Soft Tissue and Orthopaedic Surgery. Studies of naturally occurring diseases in dogs and cats by veterinarians have been invaluable for unravelling the natural history and pathogenic mechanisms involved in neurological disease.
Preventing disease in animal populations
The Referral Center for Animal Models of Human Genetic Disease (RCAM) formed in 1974 at the University of Pennsylvania, is a unique resource that excels in the discovery and characterization of genetic disease in veterinary patients. The RCAM identifies naturally occurring genetic disease through 1) clinics at the School of Veterinary Medicine of the University of Pennsylvania, 2) tissue samples submitted to the Metabolic and Molecular Laboratory; or 3) collaborations with an international network of veterinary specialists, researchers and institutions. Once the mutation responsible for the disease is identified, the next step is to develop tests for carrier and affected animals and to recommend informed breeding to remove disease from the animal population and to preserve gene pools.
Developing therapies for hereditary neurological disease
Finally, naturally occurring diseases in dogs and cats have been instrumental for the evaluation of the long-term safety and efficacy of novel therapies. In many instances, clinical trials may be performed in client-owned animals with informed consent. However, in the case of rare diseases, breeding colonies may be established to better understand disease progression, develop biochemical and imageable biomarkers of disease severity and progression, and study the safety and efficacy of novel therapies. These studies have been directly responsible for moving novel small molecule therapy, enzyme replacement therapy, and gene therapy into clinical trials in patients to improve human and animal health. An example of the usefulness of these naturally occurring diseases includes studies in the Niemann Pick disease type C1 (NPC1) cat that provided critical information on the route of delivery, scaling of dose, and adverse events of a small molecule, as well as development of surrogate biomarkers for therapeutic efficacy that would not have been feasible using the mouse model (3). These studies in the cat model accelerated the translation of this small molecule in the NPC1 mouse model to children, resulting in a multinational phase 3 clinical efficacy trial (4).
A second example includes the development of AAV-mediated gene therapy delivered at the cisterna magna to treat the previously untreatable globoid cell leukodystrophy (Krabbe disease) in the dog (5); this therapy is now being developed for use in infants. Similar preclinical trials in large animal models of the mucopolysaccharidoses and idiopathic epilepsy have resulted in planned or ongoing clinical trials in patients.
The future
Working together, veterinarians, physicians and researchers are opening new doors in the understanding of neurological disease and the development of new therapies. Through collaborative work on diseases that affect many species, cures for neurological diseases will be developed that will benefit both veterinary and human patients.
References
- Gurda BL, Bradbury AM, Vite CH. Canine and feline models of human genetic diseases and their contributions to advancing clinical therapies. Yale J Biol Med 90: 417-431, 2017. PMC5612185.
- Gurda BL, Vite CH. Large animal models contribute to the development of therapies for central and peripheral nervous system dysfunction in patients with lysosomal storage disease. Hum Mol Genet 28: R119-R131, 2019.
- Vite CH, Bagel JH, Swain GP, Prociuk M, Sikora TU, Stein VM, O’Donnell P, Ruane T, Ward S, Crooks A, Li S, Mauldin E, Stellar S, De Meulder M, Kao ML, Ory DS, Davidson C, Vanier MT, Walkley SU. Intracisternal cyclodextrin prevents cerebellar dysfunction and Purkinje cell death in feline Niemann-Pick type C1 disease. Sci Transl Med 7(276):276ra26. doi: 10.1126/scitranslmed.3010101, 2015. PMC4415615.
- Ory DS, Ottinger EA, Farhat NY, King KA, Jiang X, Weissfeld L, Berry-Kravis E, Davidson CD, Bianconi S, Keener LA, Rao R, Soldatos A, Sidhu R, Walters KA, Xu X, Thurm A, Solomon B, Pavan WJ, Machielse BN, Kao K, Silber SA, McKew JC, Brewer CC, Vite CH, Walkley SU, Austin CP, Porter FD. Intrathecal 2-hydroxy-beta-cyclodextrin decreases neurological disease progression in Niemann-Pick disease type C1: an ad hoc analysis of a non-randomized, open-label phase 1/2trial. Lancet Aug 10. pii: S0140-6736(17)31465-4. doi: 10.1016/S0140-6736(17)31465-4, 2017. PMC6176479.
- Bradbury AM, Bagel JH, Nguyen D, Lykken E, Pesayco-Salvador J, Jiang X, Swain GP, Hendricks IJ, Miyadera K, Hess RS, Ostrager A, ODonnell P, Sands MS, Ory DS, Shelton GD, Bongarzone ER, Gray SJ, Vite CH. Krabbe disease successfully treated via monotherapy of intrathecal gene therapy. J Clin Invest Volume 130, Issue 9 (September 1, 2020). PMC7456224.
Please note: This is a commercial profile