The Health Foundation analysed publicly available data to assess NHS performance and the effects of winter pressures on the health service
Historically, the NHS has faced pressure during the winter, with lower temperatures exacerbating long-term conditions like asthma and an increased risk of viruses, such as influenza and norovirus, spreading more easily. Winter also creates additional challenges for delivering health services, with staff working beyond the demands of routine care to deliver seasonal vaccinations to the public.
In a new analysis, The Health Foundation has delved into how the NHS performed during winter 2024/25, exploring the extent to which urgent and emergency care disruptions were caused by higher-than-usual levels of winter illnesses and/or systemic weaknesses within the NHS.
How did urgent and emergency care perform this winter compared to previous winters?
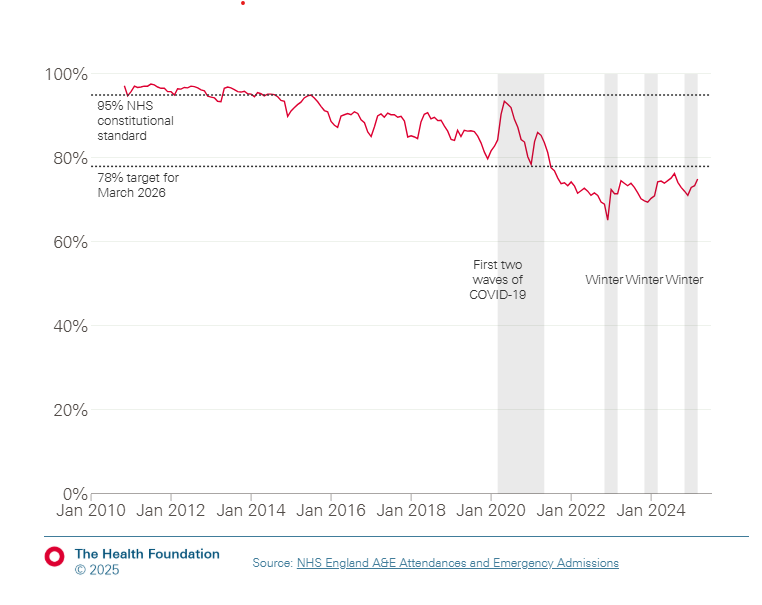
The NHS constitutional standard is that at least 95% of patients attending A&E should be admitted, discharged, or transferred within four hours of arrival.
In the 2024/25 winter, 73% of all A&E patients were seen within four hours, slightly more than in 2022/23 (70%) and 2023/24 (71%) but far below the 95% constitutional standard. Performance was even worse at central emergency departments, with less than 60% of patients treated within four hours.
The last time the NHS met the 95% standard was in the 2014/15 winter season, highlighting that performance has steadily fallen in the previous ten years.
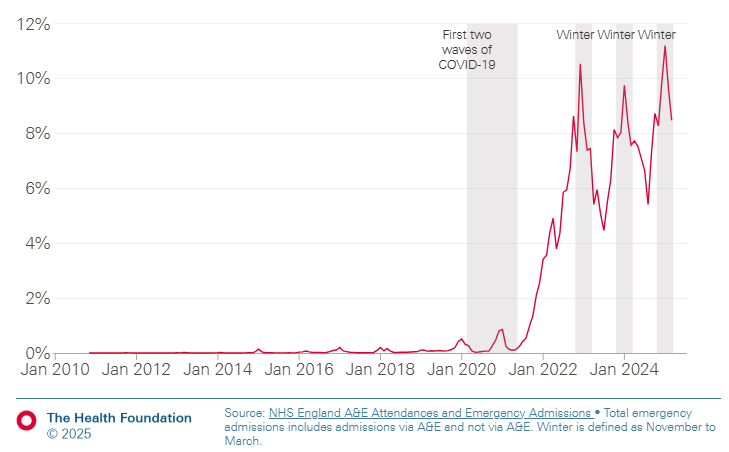
A record 11% of patients waited over 12 hours to be admitted to hospital
Since COVID-19, the NHS has reported significant increases in ‘trolley waits’ where patients wait for over 12 hours for a hospital bed after a decision to admit, usually due to a lack of available beds. In winter 2024/25, 11% of patients waited over 12 hours for a bed, compared to 9% in the past three winters.
How did levels of hospitalisations for common winter illnesses affect performance?
This winter, a record number of hospital bed days were needed for patients with flu – over 315,000 compared with around 174,000 in 2023/24 and around 211,000 in 2022/23. This is likely because the weekly admission rate peaked before Christmas at a level higher than most winters; the peak was lower than in 2022/23 but took longer to fall back to normal levels.
Admission rates to critical care were similar to the past two winters and lower than in 2018/19, suggesting flu severity was not higher than usual.
The burden of COVID-19 is easing
Weekly COVID-19 hospital admission rates have fallen considerably since the onset of the pandemic. They peaked at 11 admissions per 100,000 people per week in 2022/23 and five per 100,000 in 2023/24 but remained below two per 100,000 throughout winter 2024/25 – likely easing some of the burden on NHS services this winter.
High bed occupancy and delayed discharge strike again
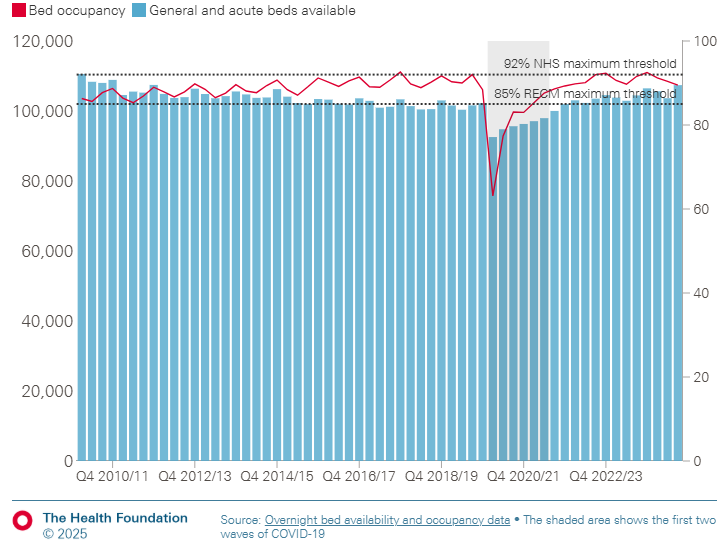
Bed occupancy has remained consistently high during winter, both before and after COVID-19.
Despite the NHS adding around 2,000 general and acute beds this winter compared to 2022/23, occupancy levels remain above the 85% safety threshold recommended by the Royal College of Emergency Medicine. Since 2010, winter occupancy has regularly exceeded this threshold, surpassing 90% in 2014/15 and the NHS’s 92% maximum target in 2017/18. Adult general and acute beds are especially affected.
The NHS continues to perform worse than before the pandemic
The analysis by The Health Foundation concluded that the NHS continues to perform worse than before the pandemic, reporting record or near-record operational problems across urgent and emergency care. These findings beg the question of what contributes to the underlying issues causing an annual winter crisis.