A new case report details a novel genetic mutation linked to drug resistance in a non-small cell lung cancer patient. Researchers identified a RUFY1-RET fusion, highlighting the need for advanced genetic testing to guide treatment strategies and combat evolving resistance
Published in the journal Oncotarget, this finding underscores the complex nature of cancer and the critical role of advanced genetic testing in guiding treatment strategies. The report, authored by Jenny L. Wu and Wade T. Iams from Vanderbilt University School of Medicine and Vanderbilt-Ingram Cancer Center, highlights the importance of ongoing monitoring for genetic changes that can lead to resistance to targeted therapies.
The new case report details a novel genetic mutation linked to drug resistance in a non-small cell lung cancer patient and how evolving drug resistance is continuing to cause researchers issues.
Initial success and subsequent drug resistance
The patient, a 42-year-old non-smoker, was initially diagnosed with stage IV NSCLC harboring a CD74-ROS1 gene fusion. This specific genetic alteration made his cancer susceptible to lorlatinib, a targeted therapy. For six months, the patient responded positively to the treatment. However, his condition eventually progressed, indicating the development of drug resistance.
Unveiling the novel mutation
To understand the cause of this resistance, clinicians employed RNA next-generation sequencing (RNA NGS). This sophisticated testing method revealed a previously unidentified genetic change: a RUFY1-RET fusion. This novel mutation is believed to be the key factor driving the cancer’s resistance to lorlatinib. The discovery highlights the power of RNA NGS in detecting mutations that might be missed by more conventional DNA-based testing.
A combined approach and future implications
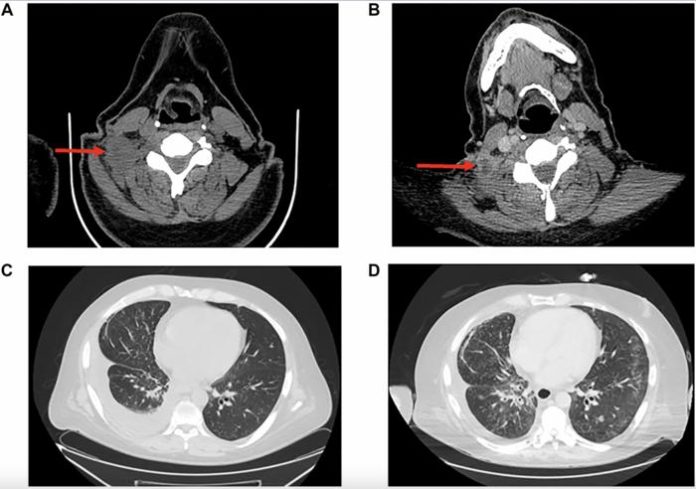
Following the identification of the RUFY1-RET fusion, the patient’s treatment plan was adjusted to include a combination of lorlatinib and pralsetinib. Pralsetinib is a drug specifically designed to target RET gene alterations. This combined therapy initially showed promise, leading to a decrease in tumor size and fluid accumulation around the lungs, as documented by CT scans. However, the benefits of this combination were unfortunately short-lived, lasting only about four months before the cancer progressed again.
The significance of the finding
This case represents the first reported instance of a RET fusion acting as a potential mechanism of resistance to lorlatinib in NSCLC. Furthermore, it identifies RUFY1 as a novel RET fusion partner.
The authors emphasise the importance of comprehensive genetic testing, including both DNA and RNA analysis, at the time of disease progression in patients with cancers driven by targetable oncogenic drivers. This approach allows clinicians to identify acquired resistance mutations, which can inform treatment decisions.
A stepping stone for future research
While the combined therapy in this particular case provided only temporary relief, it offers valuable insights for future research and patient care. Understanding the mechanisms of drug resistance is crucial for developing more effective treatment strategies.
This case underscores the need for ongoing research into combination therapies and novel approaches to combat drug resistance in NSCLC. By identifying and understanding these rare mutations, researchers and clinicians can work towards developing more durable and personalized treatments for patients facing this challenging disease. The case serves as a reminder of the dynamic nature of cancer and the constant need for innovation in cancer treatment.