A landmark study presented at ESCMID Global 2025 reveals the devastating impact of antimicrobial resistance (AMR) on children’s health. In 2022, over 3 million children worldwide died from antibiotic-resistant infections, highlighting the urgent need for global action
Over 3 million children globally lost their lives in 2022 due to infections that were resistant to antibiotic treatment.
The groundbreaking study, unveiled at ESCMID Global 2025, emphasises the urgent need for both regional and global strategies to combat paediatric AMR, particularly in regions with high burdens, such as South-East Asia and Africa.
Pediatric AMR crisis
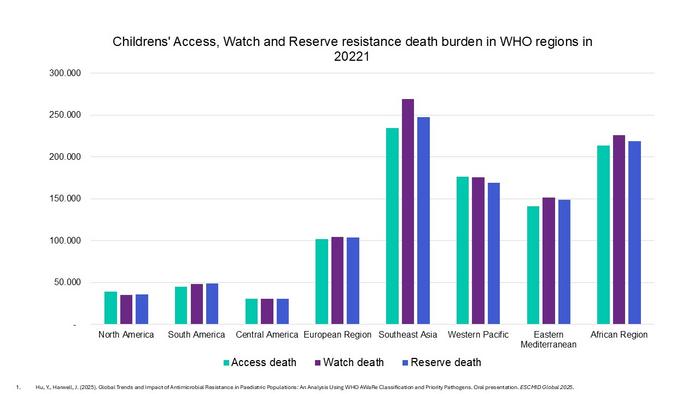
Children are especially vulnerable to infections, and AMR poses a significant threat to their well-being. The study highlights that access to new antibiotic formulations is often more limited for children due to delays in product development. The data reveals alarming statistics: in 2022, over 752,000 children in Southeast Asia and 659,000 children in Africa died from complications associated with AMR. A significant portion of these deaths was linked to the use of “Watch” and “Reserve” antibiotics.
The dangers of Watch and Reserve antibiotics
The study found that many of these deaths were linked to the increased use of Watch and Reserve antibiotics. Watch antibiotics carry a high risk of resistance, while Reserve antibiotics are last-resort treatments for severe, multidrug-resistant infections. These antibiotics are not intended for first-line treatment.
Between 2019 and 2021, the use of Watch antibiotics surged by 160% in Southeast Asia and 126% in Africa. Similarly, Reserve antibiotic use increased by 45% in Southeast Asia and 125% in Africa. Globally, out of the 3 million children’s deaths, 2 million were associated with the use of Watch and Reserve antibiotics.
Professor Joseph Harwell, a study co-author, warned, “While the rise in use of Watch and Reserve antibiotics may be necessary in response to the concurrent rise in drug-resistant infections, the sharp rise in use of these drugs presents several serious long-term risks. Their increased use, especially without careful oversight, elevates the risk of resistance and limits future treatment options. If bacteria develop resistance to these antibiotics, there will be few, if any, alternatives for treating multidrug-resistance infections.”
Factors fueling AMR
Several factors contribute to the severity of AMR, especially in low- and middle-income countries. These include:
- Overcrowded hospitals
- Poor sanitation
- Weak infection prevention measures
- Lack of diagnostic tools
- Overuse and misuse of antibiotics
- Absence of effective national surveillance and antimicrobial stewardship programs
These conditions facilitate the spread of resistant pathogens within healthcare settings and communities, making it difficult to track resistance trends and implement effective treatment protocols.
An urgent call to action
The study emphasises that rising resistance to Watch and Reserve antibiotics will lead to higher treatment failure and increased mortality rates, particularly in low- and middle-income countries with limited access to alternative treatments.
Professor Harwell stressed the need for urgent and coordinated action at both regional and global levels. He called for adopting a “One Health” approach in global and national AMR surveillance, with cost-effective systems to inform treatment guidelines and measure the impact of control interventions.
He also urged policymakers to mandate hospital-based antimicrobial stewardship programs in all paediatric healthcare facilities and to improve age classifications in surveillance data. National guidelines are needed to ensure that routine surveillance informs antibiotic use.