Why starting at the beginning is so important in paediatric haematology research in the UK is a point impressed on us by Dr Sujith Samarasinghe at Great Ormond Street Hospital, London and Grazina Berry, CEO of the Aplastic Anaemia Trust
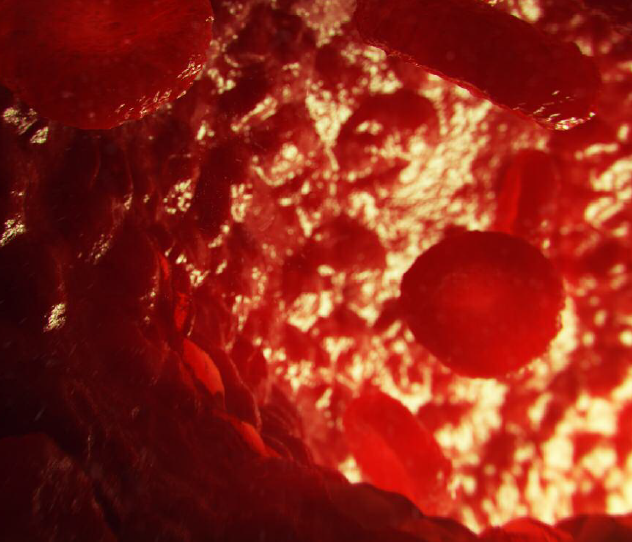
The current landscape in paediatric aplastic anaemia research and treatment in the UK is
quite complex. Huge strides have been made in the treatment of children with the rare bone marrow failure across 20 + treatment centres, primarily via bone marrow transplantation in acquired cases of AA or immunosuppressive therapy. This has helped build an excellent reputation for successful treatment of children with aplastic anaemia, both acquired and inherited, at key centres in the UK including Great Ormond Street Hospital, St Mary’s Hospital in London, or in Newcastle, Manchester, Birmingham and other major treatment centres, as well as beyond.
However, what’s been lacking is answers to some fundamental yet basic questions:
- What is the prevalence and incidence of childhood aplastic anaemia in the UK?
- What are the numbers of constitutional versus acquired, very severe, severe and moderate cases?
- What are the outcomes of different treatment
options and what might the Quality of Life measures
tell us about the experiences of children and families dealing with the disease?
These and many other questions will be answered by a brand new research project to establish UK’s first paediatric bone marrow failure registry and biobank starting in 2019 and led by Dr Sujith Samarasinghe at Great Ormond Street Hospital in London, who is working collaboratively with colleagues in Manchester, York and Oxford University. Funded by the Aplastic Anaemia Trust over a three-year period, the project will enable the collection of a range of data from 30 newly diagnosed patients per year, including chromosomal breakage results, telomere lengths, molecular genomics results, first-line treatment received and subsequent outcomes.
The parents of children diagnosed with aplastic anaemia, a rare and life-threating auto-immune disease, face huge uncertainties in terms of diagnosis, treatment and recovery pathway currently. This is in addition to a hefty emotional trauma, significant life changes that the entire family has to brace itself for, in preparation for and during a lengthy, exhausting and expensive treatment, recovery and transition back to a new normality.
A mum of a 15-month old baby diagnosed with AA says: “We didn’t understand at first why we went straight to transplant. We didn’t know there may have been other treatment options”.
According to Dr Samarasinghe, the benefits of the study to the UK paediatric haematology as well as the patient community will be significant, as he explains in his own words “We’ll have a much better understanding of the causes of AA. This could lead to the discovery of
novel genes that lead to childhood aplastic anaemia. We’ll also be closer to understanding the role of the immune system in acquired childhood AA. In addition, we will obtain a much deeper understanding of the lived experience and psycho-social impacts of these rare conditions on these patients’ wider lives”.
Dr Sujith Samarasinghe
Great Ormond Street Hospital, London
Tel: +44 (0)20 7405 9200
www.gosh.nhs.uk
www.twitter.com/GreatOrmondSt
Grazina Berry
CEO
Aplastic Anaemia Trust
Tel: +44 (0)7748 186 858
support@theaat.org.uk
www.theaat.org.uk
www.twitter.com/AplasticAnaemia