Nicola Hemmings, Workplace Scientist at Koa Health, and Dr Claire Vowell, Counselling Psychologist, discuss the growing problem of burnout among government healthcare workers, and address what organisations can do to mitigate burnout risk
Workplace stress is something many of us view as unavoidable. Too often, we think of it as part and parcel of having busy professional and personal lives and caring about outcomes and results. But when work-related stress persists without relief, it can lead to burnout. And burnout is bad news for both individual and organisational health.
According to the World Health Organisation, burnout is an occupational phenomenon (not a medical condition) with three defining characteristics: feelings of emotional exhaustion, cynicism towards work, and reduced professional efficacy[1]. But what makes burnout different from being very stressed or very tired or both?
Is it stress or burnout?
Unlike burnout, stress comes and goes and can usually be traced to a source, be it a situation or a person. Work-based stress is typically caused by the imbalance of demands and resources available to deal with them[2]. People who are stressed at work can usually imagine feeling better once their circumstances return to normal. However, individuals suffering from burnout often have trouble feeling positive about how things will go at work in the future.
Burnout is workplace specific
Its causes and symptoms impact functioning well at work[3]. Organisational risk factors for burnout include the following:
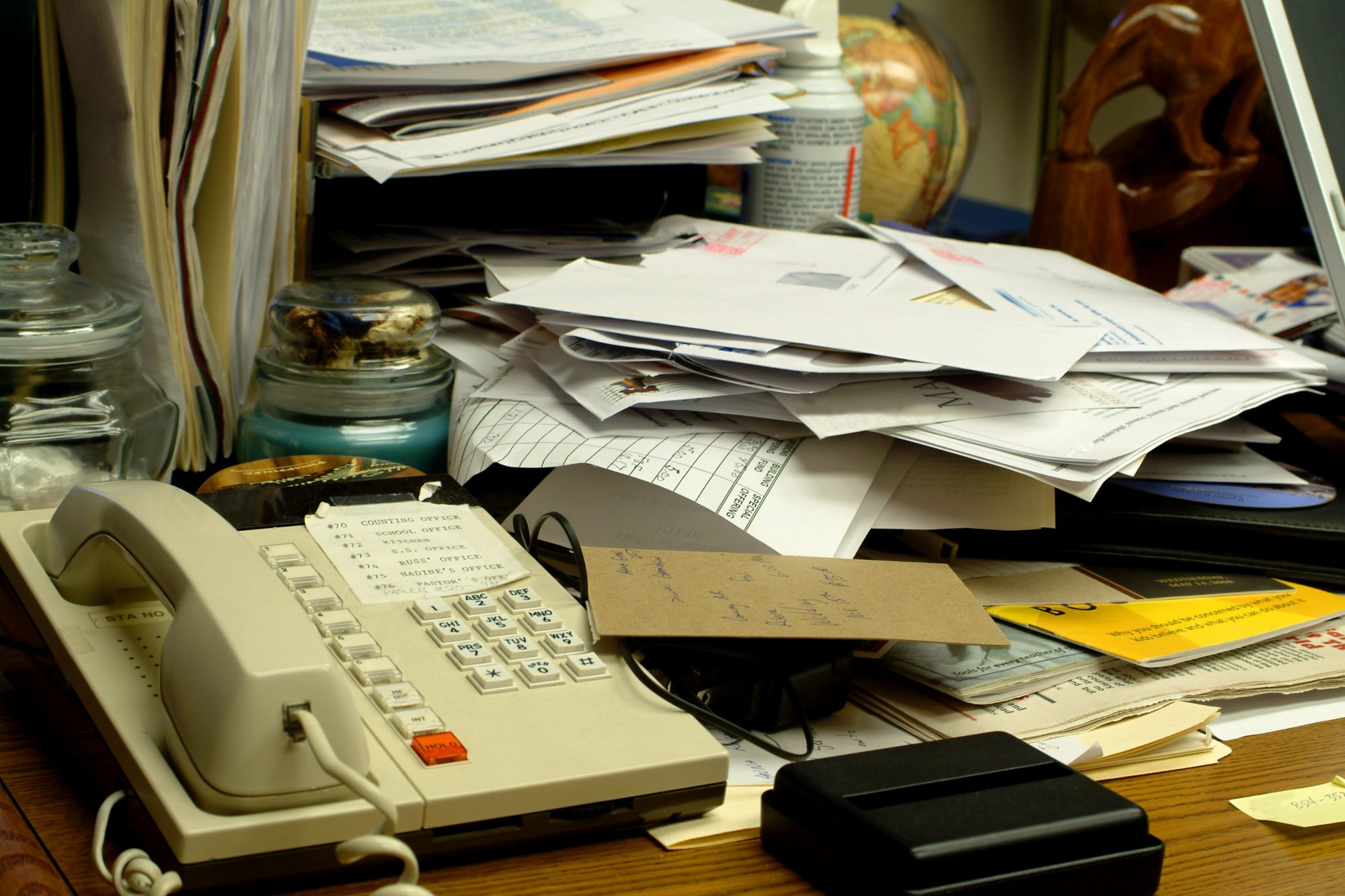
- A heavy workload and an overload of demands
- A lack of control and autonomy
- Insufficient support from peers or managers
- Relational conflict
- Lack of role clarity or clear objectives
- Constant change or poor communication of change
While burnout has many symptoms in common with stress, its impacts are longer-lasting, in regards to both mental and physical health, as well as organisational outcomes[4].
Burnout is a predictor of physical health problems, including high cholesterol, type 2 diabetes, heart disease, musculoskeletal pain, and even increased mortality risk under 45 years of age[5]. Possible psychological health issues include insomnia, depressive symptoms, use of psychotropic and antidepressant medications, and hospitalisation for mental illness.
In the work environment, burnout is linked to absenteeism, increased turnover, new disability claims, and increased workplace errors[6]. Each has a cost impact, for example training new NHS staff ranges between £75K to train a new support staff member and £245K for a new doctor[7]. In addition, workplace errors in medication cost upwards of £98M and more than 1,700 lives yearly[8].
Healthcare workers are at higher risk for burnout
Chronic excessive workload in the NHS has been worsened by staff shortages, the constant changes of the pandemic, and insufficient support. This is resulting in burnout, impacting healthcare workers and the patients they’ve dedicated their lives to caring for.
On top of the many health risks healthcare workers endure, burnout can also interfere with medical staff’s ability to provide compassionate, competent care. High levels of stress are linked to medical and nursing errors, lower patient satisfaction, and poorer care quality[9].
It is therefore essential for healthcare workers, the patients they care for, and the success of the NHS system as a whole to address and prevent burnout.
There are simply too many demands on the limited resources workers have available. The challenge the NHS faces is redesigning ways of working to better resource care, taking into account staff’s elevated emotional and physical workloads. However, organisational change takes years. In the meantime, fast, effective action is required to support individuals working in the healthcare system.
Facilitating burnout prevention
Healthcare organisations need scalable, evidence-based mental health tools to support workers where they’re at. Digital-first solutions can help organisations ensure their health care workers have the resources they need to take care of their health and wellbeing, whenever and wherever they need them.
Many health care workers aren’t comfortable speaking about their mental health struggles at work[10]. To reduce the barriers to asking for help, organisations could consider using external, independent services that staff can access 24/7 to support their mental wellbeing and get discreet, in-the-moment help. Ideally, these services are flexible, fitting in with healthcare workers’ daily life and demands.
While organisations work on updating their approach to employee wellbeing, digital-first mental health solutions can help support individuals. Mobile-based resources can support busy health professionals with limited friction, allowing them to access support on their own terms.
But more than easy-to-access, these resources must also be secure, ethical, independently reviewed, backed by standard testing protocols, and based on clinically validated techniques. Techniques validated in clinical practices (such as those from cognitive behavioural therapy or CBT) have been shown to be effective when delivered via an app[11]. For example, in the first RCT (randomised control trial) of our science-based mental wellbeing app, Koa Foundations, we saw a positive effect on measures of overall wellbeing, sleep, and anxious thoughts after only two weeks of use.
But no one tool can solve the problem of burnout—offering practical resources to support healthcare workers’ mental health is just the beginning. In order to truly support mental health for all (healthcare workers), the NHS and its partnering organisations will need to make changes to organisational culture and tackle existing pain points such as staff shortage and chronic excessive workload.
Inspiring organisational change
Addressing burnout is one piece of a much bigger picture: how organisations can take better care of mental health and wellbeing for essential healthcare workers. Recognising that a problem exists is the first step, but large-scale change takes time, and let’s face it, plenty of work.
That said, there are certain small actions with the potential to make a big impact on mental wellbeing in almost any workplace.
- Check in with employees
- Build in appropriate time during shifts to ask employees how they’re doing. Pay attention to their answers, and make it clear that you (and your organisation) genuinely care. Follow up with words of encouragement, advice on accessing helpful resources, or even just a second question like ‘what would be most helpful to you right now?’ or ‘how can I best support you?’.
- Provide the right mental health resources (and time to use them)
- To ensure that workers prioritise mental health and wellbeing, organisations must provide tools and benefits that make seeking support simple, properly signpost said resources, and then ensure that workers also have the time to use them.
- Role model healthy behaviour
- Building a culture of wellbeing takes time. It starts with showing and encouraging the behaviours needed to create a supportive culture. Look out for others, take full work breaks or holiday time where possible to rest and recover. If suitable, share current struggles to break the stigma of talking about tough challenges. Data[12] shows that when leaders at an organisation are willing to be vulnerable, it improves employee trust and employee trust is key to creating a culture where people feel like they can ask for help when they need it.
Does your organisation need help to build a culture that protects and prioritises employee mental health? With resources at clinics and hospitals increasingly challenging to access, it may be time to bring in some outside reinforcements. Koa Health can help. Koa Health can help. Contact us at support@koahealth.com.
About Koa Health
Koa Health is a leading global provider offering evidence-based, personalised, integrated solutions that deliver mental health for all. Available to more than 3 million users worldwide, Koa Health leverages deep clinical expertise, research, and technology to deliver practical and accessible support that adapts to people’s unique circumstances, leading to lasting behavioural change and positive mental health outcomes.
About the authors
Nicola Hemmings has over a decade of experience applying an evidence-based approach to workplace performance. A workplace scientist and content creator at Koa Health, she’s committed to finding evidence-based solutions to real-world problems in the workplace and beyond.
Dr Claire Vowell is a counselling psychologist who’s passionate about improving access to mental health care. In her work at Koa Health, she leverages clinically validated techniques to create interventions to improve people’s mental wellbeing.
References
[1]https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
[2]https://www.semanticscholar.org/paper/An-empirical-examination-of-self-reported-work-U.S.-Cavanaugh-Boswell/626c9dbce3154e001994bd0d5180463677cb07d4?p2df
[3] https://www.hse.gov.uk/stress/standards/index.htm
[4] https://www.ncbi.nlm.nih.gov/books/NBK279286/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5627926/
[6] https://www.tandfonline.com/doi/abs/10.1080/13548500903311554; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5627926/
[7] https://www.charitytoday.co.uk/nhs-staff-exodus-to-cost-government-21-7billion/
[8] https://www.bmj.com/company/newsroom/237-million-medication-errors-made-every-year-in-england/
[9] https://www.kingsfund.org.uk/blog/2021/06/
naming-issue-chronic-excessive-workload-nhs;
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8237033/; https://med.stanford.edu/news/all-news/2018/07/medical-errors-may-stem-more-from-physician-burnout.html
[10]https://cdn.mentalhealthatwork.org.uk/wp-content/
uploads/2021/02/02114357/BMA-Stigma-Resource-.pdf
[11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3584580/
[12]https://hbr.org/2014/12/what-bosses-gain-by-being-vulnerable
*This is a commercial profile.
© 2019. This work is licensed under CC-BY-NC-ND.











