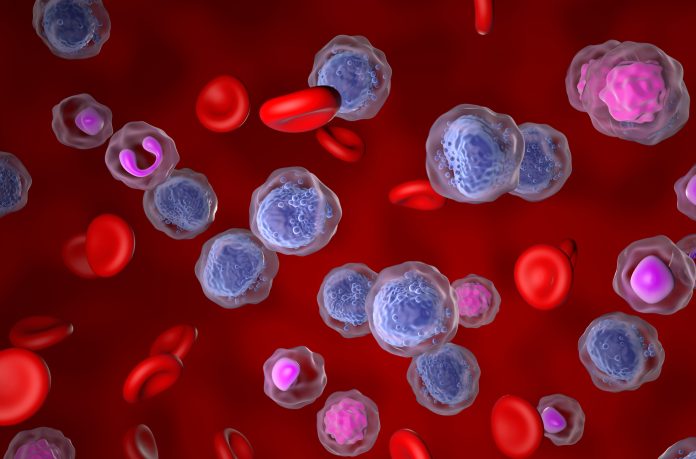
Chronic lymphocytic leukemia (CLL) is a B-cell malignancy, with disease progression ranging from slow and indolent to aggressive
Although treatments have improved, CLL is still incurable, and the disease is still not fully understood.
Understanding CLL progression
CLL often links to autoimmune complications, which means clinical trials have usually had poorer outcomes. This is why it’s important to understand the relationship between autoimmunity and CLL progression, as these autoimmune complications could work to the advancement of the disease.
Recent research using a mouse model that expresses an active Receptor Activator of NF-κB (RANK) in B cells (RK mice) has revealed new insights into this connection.
It was revealed that these mice develop autoimmune manifestations that mimic the ones shown in human CLL. This included the production of anti-nuclear antibodies and glomerulonephritis.
Autoimmune features develop concurrently with CLL-like disease in B1 B cells, indicating that the autoimmune environment may influence disease progression.
When analysing RK-driven leukemic cells, the researchers found that these cells showed a less aggressive form of CLL than the classic TCL1 model, which is another common mouse model used for analysing CLL.
The researchers found CLL heterogeneity and suggested that the immune environment in RK mice might modulate the disease progression uniquely.
A further examination of the B cell receptors (BCRs) of both plasma cells and CLL cells showed some similarities in their CDR3 regions, suggesting that both conditions may arise from a shared progenitor cell.
This shared origin suggests that it could be an antigen-driven process that is fuelling both autoimmunity and CLL, suggesting that the immune system’s recognition of certain antigens may underlie the development of autoimmune disease and malignant transformation in CLL.
The relationship between autoimmunity and CLL progression
Having looked deeper into the role of Blimp-1, a protein that regulates plasma cell differentiation, it further shows the complex relationship between autoimmunity and CLL progression.
Deleting Blimp-1 in the RK mice initially enhanced the formation of B1 cells and accelerated the development of CLL in younger mice.
However, as the mice aged, the elision of Blimp-1 nearly halted CLL progression. This suggests that while plasma cell differentiation and the associated autoimmune responses can drive CLL development early on, they might have a more suppressive role in the advanced stages of the disease, pointing to a dynamic and shifting relationship between autoimmunity and leukemia.
Treating CLL in the future
The findings from this study are important because they show how autoimmune complications in CLL are not just a byproduct of the disease but may actively influence its progression.
Specifically, the plasma cell-mediated autoimmunity in RK mice creates an inflammatory environment that might accelerate the disease process.
This insight could open new areas for targeted therapies that aim to modulate the immune response to slow or halt CLL progression.
Therapies targeting BCR signalling pathways, such as Bruton tyrosine kinase (BTK) inhibitors or phosphoinositide 3-kinase (PI3K) inhibitors, have already shown promise in treating CLL and its associated autoimmune complications. These treatments not only address the malignant B cells but also help control the autoimmune manifestations, suggesting that a dual approach targeting both aspects of the disease may improve patient outcomes.
Overall, the connection between autoimmunity and CLL is complicated and likely contributes to the disease’s progression. The research using the RK mouse model emphasises the importance of understanding this connection, as it may reveal new therapeutic strategies that target the disease’s autoimmune and leukemic components.