Jennifer J. McComas, PhD and Alefyah Shipchandler from the University of Minnesota discuss the current state of the evidence for communication intervention for individuals with Rett syndrome
Researchers who investigate habilitative treatments for severe neurodevelopmental disorders rely on human participants agreeing to serve as the subjects of our experiments. Some families consent to participate because they have experienced something like this: they gave birth to a healthy baby and watched that baby hit developmental milestones for the first six or more months of life, only to observe their child, who has developed fine motor and some early vocal language, go through a period of regression in which they lose motor and communication skills.
Without motor and communication skills, it is nearly impossible to know their cognitive abilities, but most experts report cognition is also severely impaired. Although this condition is rare, affecting approximately one in 10,000 girls born worldwide (it is exceedingly rare in boys), it is nevertheless devastating. The neurodevelopmental disorder, now known as Rett syndrome (RTT), was first described by an Austrian pediatrician1, but for decades, individuals with RTT were misdiagnosed as having autism due to similarities in behavioural phenotype2. In 1999, Huda Zoghbi and her colleagues discovered that genetic mutations in the gene MECP23,4, located on the X chromosome, cause RTT. Systems that experience impairment often include speech, motor skills, breathing, cardiac function, chewing, swallowing and digestion.
Although extensive research on the genetic basis and medical treatments for RTT in non-human populations has occurred in the past 20 years5,6,7,8, the goal of that research has been a better understanding of the causal mechanisms, potential treatments and cures for the disorder. Far less experimental research has been conducted in the area of treatment of communication deficits. Yet, while families wait for effective treatment of symptoms or a cure, they are in need of empirically validated interventions that will allow their daughters with RTT to communicate their wants and needs.
Persons with multiple disabilities, including severe physical and communication disabilities, often need assistive technology in the form of augmentative and assistive communication (AAC) devices to communicate. Eye-gaze technology that involves an eye-tracking device and a computer-based programme that produces vocal output is an emerging technology for individuals with severe motor impairments9 and is increasingly recommended for individuals with RTT10, 11, 12.
Despite claims of individuals with RTT using eye-gaze technology to converse with their families12 and to read13, there is little published empirical evidence of effective use of eye-gaze devices by individuals with RTT. As such, the National Institute on Deafness and Other Communication Disorders (NIDCD) within the National Institutes of Health (NIH) in the United States, funded our research project designed to develop a reinforcement-based intervention model for addressing the complex communication needs in RTT. As part of that project, we examined the published peer-reviewed empirical literature on the use of a behavioural intervention to teach or improve communication of individuals with RTT and our findings were somewhat surprising.
A systematic search was conducted in the following electronic databases: PsychINFO, PubMed and Academic Search Premier. In all databases, “Rett syndrome” was inserted into the search field along with one of the following: “behavioural + intervention,” “communication + intervention,” “educational + intervention,” “habilitative + intervention,” and “augmentative communication,” for a total of five search term pairs.
From the resulting 310 publications, chapters, non-peer-reviewed papers (e.g., dissertations) and non-English articles were excluded. In addition, articles that focused on genetics, reports of general characteristics of RTT, medical interventions and interventions conducted with non-human subjects were excluded. Finally, any article in which communication was not reported as a dependent variable or that did not describe a procedure related to teaching or improving a communicative response was excluded. A total of 15 studies were identified for evaluation.
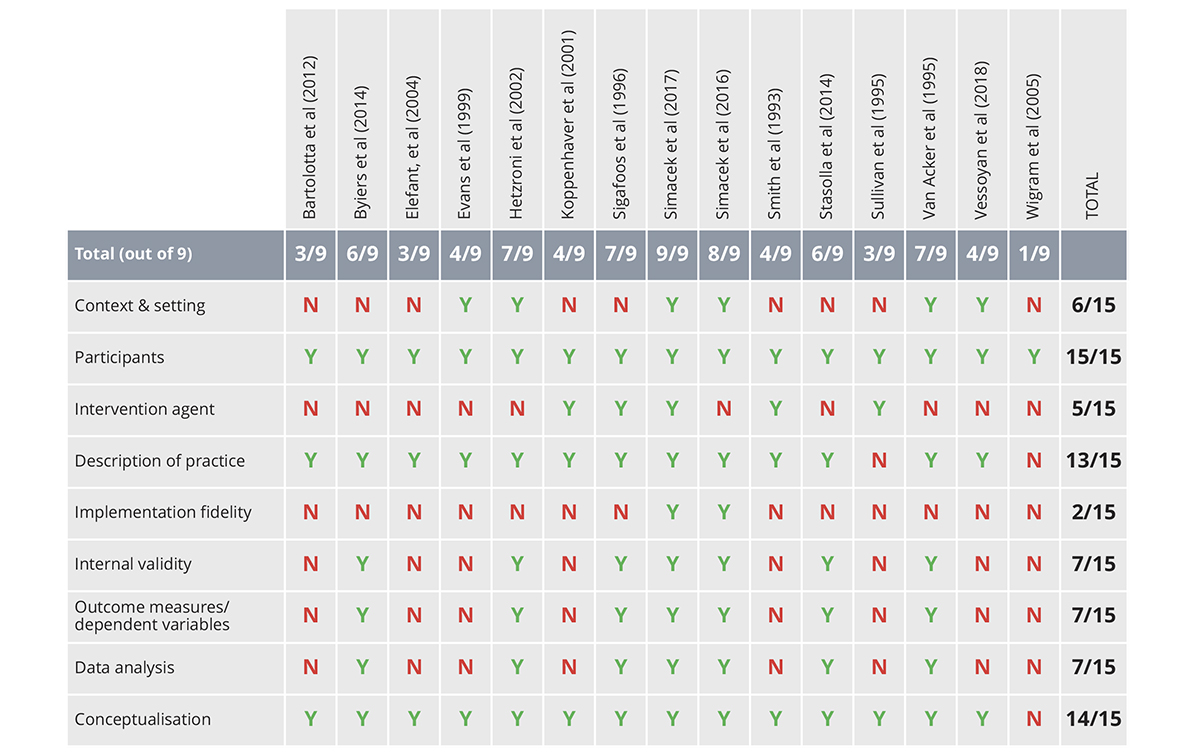
Next, we evaluated each of the 15 studies using the Council for Exceptional Children (CEC): Standards for Evidence-Based Practice in Special Education14. In addition, an indicator of conceptualisation underlying the study15 was included in the review. The CEC’s standards for evidence-based practice contain sub-features of each indicator. For an indicator to be considered “met,” the study needed to address all the relevant sub-features of the indicator. For example, quality indicator five ‘Implementation Fidelity’ includes three sub-features pertaining to adherence, dosage and duration14. For an indicator to be scored as Yes (Y), all sub-features needed to be adequately addressed. One rater independently evaluated all 15 articles according to the CEC standards, and a second rater independently evaluated eight of the 15 articles using the same criteria. Inter-rater agreement for the nine indicators was 100% across all articles that were evaluated by both raters.
All 15 studies addressed non-vocal forms of communication and targeted either motor responses or eye gaze as their target behaviours, with some including both. Target communicative responses included unaided responses (e.g., signs, gestures) or technology aided responses that involved either low technology (e.g. pictures, microswitches, 2D symbols, 3D objects) or high technology (e.g., speech generating devices [SGD] activated by eye-gaze). Of the fifteen studies, two studies utilised eye-gaze technology 16, 17.
Results of the evaluation of the nine quality indicators for evidence-based practice described by the CEC (#1-8) and research described by Gersten and colleagues (#9) are presented in Table 1. The ratings of the quality indicators varied widely across the 15 studies. All 15 studies met the criteria for describing participants, all but one met the criteria for conceptualisation and all but two met the criteria for describing the practice. Only one study met the criteria for all nine indicators18 and 1/3 of the studies (five of 15) met the criteria for at least seven of the nine indicators. Four studies (1/4) met criteria for three or fewer of the nine indicators.
In our experience, families affected by RTT have been exceptionally generous with their time and energy in voluntarily participating in research projects, despite the challenges they encounter caring for a loved one with severe multiple disabilities. As researchers, we owe it to these families and to our science to conduct rigorous investigations and disseminate our procedures and results in a way that is replicable by other researchers. In our role as reviewers for publication outlets and funding recommendations, we must take stock of the body of evidence and demand continuous improvement in the quality of evidence pertaining to treatment for critical skills such as communication.
In summary, within the body of work to date, the claims vary widely pertaining to the utility of high-technology devices that involve eye-gaze for individuals with RTT. As the field matures, more studies that meet the quality standards of evidence-based practices and research and that improve understanding for whom and under what conditions particular technologies and practices are effective are imperative for continued progress in the field 19, 20.
The research described in this profile is supported by the National Institute on Deafness and Other Communication Disorders (NIDCD/NIH) Grant No. 1R21DC015021-01A1.
References
Note: * Indicates the article was included in the review
1 Rett, A. (1966.) [On an unusual brain atrophy syndrome in hyperammonemia in childhood]. Wein Med Wochenschr, 116, 723-6.
2 Percy, A. K. (2011). Rett Syndrome: Exploring the Autism Link. Archives of Neurology, 68, 985-989. http://doi.org/10.1001/archneurol.2011.149.
3 Amir, E. R., Van Den Veyve,r B. I., Wan, M.,Tran, Q. C., Francke, U., & Zoghb,i Y. H. (1999). Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genetics, 23(2), 185-8.
4 Nuzzo, R. (2006). Profile of Huda Y. Zoghbi. Proceedings of the National Academy of Sciences of the United States of America, 103, 3017-3019. http://doi.org/10.1073/pnas.0509604103.
5 Gogliotti, R., Senter, R., Fisher, N., Adams, J., Zamorano, R., Walker, A.,… Niswender, C. (2017). MGlu potentiation rescues cognitive, social, and respiratory phenotypes in a mouse model of Rett syndrome. Science Translational Medicine, 9, 1-11.
6 Ghorbel, R., Fendri-Kriaa, R., Ben Salah, N., Belguith, G., Ammar-Keskes, N., Rouissi, L.,… Fakhfakh, N. (2018). First report of an unusual novel double mutation affecting the transcription repression domain of MeCP2 and causing a severe phenotype of Rett syndrome: Molecular analyses and computational investigation. Biochemical and Biophysical Research Communications, 497, 93-101.
7 Na, S. E., Morris, J.M., Nelson, D. E, & Monteggia, M. L. (2014). GABAA Receptor Antagonism Ameliorates Behavioral and Synaptic Impairments Associated with MeCP2 Overexpression. Neuropsychopharmacology, 39, 1946-1954.
8 Percy, A. K., Lane, J., Annese, F., Warren, H., Skinner, S. A., & Neul, J. L. (2018). When Rett syndrome is due to genes other than MECP2. Translational Science of Rare Diseases, 3, 49-53. http://doi.org/10.3233/TRD-180021.
9 Borgestig, M., Sandqvist, J., Parsons, R., Falkmer, T., & Hemmingsson, H. (2015). Eye Gaze Performance for Children with Severe Physical Impairments Using Gaze-Based Assistive Technology – a Longitudinal Study. Assistive Technology, 28, 93-102.
10 Djukic A., & McDermott V.M., (2012). Social Preferences in Rett Syndrome. Pediatric Neurology, 46, 240-242.
11 International Rett Syndrome Foundation n.d. https://www.rettsyndrome.org/about-rett-syndrome/communication.
12 LaRiviere, J. A. (2015). Eye gaze technology for girls with Rett syndrome: From trials to conversations. Closing the Gap newsletter, 4-13. http://www.dbmhresource.org/uploads/2/2/5/7/22571778/closing_the_gap_lariviere_eye_gaze_december_2014_1.pdf [Accessed August 28, 2018].
13 Fabio, R., Castelli, I., Marchetti, A., & Antonietti, A. (2013). Training communication abilities in Rett Syndrome through reading and writing. Frontiers in Psychology, 4, 911.
14 Cook, B., Buysse, V., Klinger, J., Landrum, T., McWilliam, R., Tankersley, M., Test., D. Council for Exceptional Children: Standards for Evidence-Based Practices in Special Education. (2014). Teaching Exceptional Children, 46, 206-212.
15 Gersten, R., Fuchs, L., Compton, D., Coyne, M., Greenwood, C., & Innocenti, M. (2005). Quality Indicators for Group Experimental and Quasi-Experimental Research in Special Education. Exceptional Children, 71, 149-164.
16 Simacek, J., Reichle, J., & McComas, J. (2016). Communication Intervention to Teach Requesting Through Aided AAC for Two Learners With Rett Syndrome. Journal of Developmental and Physical Disabilities, 28, 59-81.
17 Vessoyan, K., Steckle, G., Easton, B., Nichols, M., Mok Siu, V., & Mcdougall, J. (2018). Using eye-tracking technology for communication in Rett syndrome: Perceptions of impact. Augmentative and Alternative Communication, 1-12. DOI: 10.1080/07434618.2018.1462848.
18 Simacek, J., Dimian, F. A., & McComas, J. J., (2017). Communication Intervention for Young Children with Severe Neurodevelopmental Disabilities via Telehealth. Journal of Autism and Developmental Disorders, 47, 744-767.
19 Chen, S-H. K., & O’Leary, M. (2018). Eye Gaze 101: What Speech-Language Pathologists Should Know About Selecting Eye Gaze Augmentative and Alternative Communication Systems.
20 Townend, G., Peter, M., Smeets, E., Berg, R., Berg, M., & Curfs, L., (2016). Eye Gaze Technology as a Form of Augmentative and Alternative Communication for Individuals with Rett Syndrome: Experiences of Families in The Netherlands. Journal of Developmental and Physical Disabilities, 28, 101-112.
*Bartolotta, T., & Remshifski, P. (2012). Coaching Communication Partners: A Preliminary Investigation of Communication Intervention During Mealtime in Rett Syndrome. Communication Disorders Quarterly, 34, 162-171.
*Byiers, J. B., Dimian, A., & Symons, J. F. (2014). Functional Communication Training in Rett Syndrome: A Preliminary Study. American Journal on Intellectual and Developmental Disabilities, 119, 340-350.
*Elefant, C., & Lotan, M. (2004). Rett Syndrome: Dual Intervention – Music and Physical Therapy. Nordic Journal of Music Therapy, 13, 172-182. 10.1080/08098130409478114.
*Evans, I., & Meyer, L. (1999). Modifying adult interactional style as positive behavioural intervention for a child with Rett syndrome. Journal of Intellectual and Developmental Disability, 24, 191-205.
*Hetzroni, O., Rubin, C., & Konkol, O. (2002). The use of assistive technology for symbol identification by children with Rett syndrome. Journal of Intellectual and Developmental Disability, 2002, 27, 57-71.
*Kopperhaver, A. D., Erickson A. K., Harris, B., McLellan, J., Skotko, S. B., Newton, A. R. (2001). Storybook-based communication intervention for girls with Rett syndrome and their mothers. Disability and Rehabilitation, 23, 149-159.
*Sigafoos, J., Laurie, S., & Pennell, D. (1996). Teaching children with Rett syndrome to request preferred objects using aided communication: Two preliminary studies. Augmentative and Alternative Communication, 12, 88-96.
*Smith, T., Kleystrand, M., Lovaas, O. (1993) Behavioral treatment of Rett’s disorder: Ineffectiveness in three cases. American Journal of Mental Retardation, 100, 317-22.
*Stasolla, F., De Pace, C., Damiani R., De Leone, A., Albano, V., & Perilli, V. (2014). Comparing PECS and VOCA to promote communication opportunities and to reduce stereotyped behaviours by three girls with Rett syndrome. Research in Autism Spectrum Disorders, 8, 1269-1278.
*Sullivan, M., Laverick, W., & Lewis, D. (1995). Brief report: Fostering environmental control in a young child with Rett syndrome: A case study. Journal of Autism and Developmental Disorders,25, 215-221.
*Van Acker, R., & Grant, H S. (1995). An Effective Computer-Based Requesting System for Persons with Rett Syndrome. Journal of Childhood Communication Disorders,16, 31-38.
*Wigram, T., & Lawrence, M. (2005). Music therapy as a tool for assessing hand use and communicativeness in children with Rett Syndrome. Brain and Development, 27, S95-S96.
Jennifer J. McComas, PhD
Professor
University of Minnesota
Tel: +1 612 624 5854
www.cehd.umn.edu/edpsych/people/jmccomas/
Alefyah Shipchandler
Ph.D. student
University of Minnesota
Tel: +1 612 624 5854
Please note: this is a commercial profile.