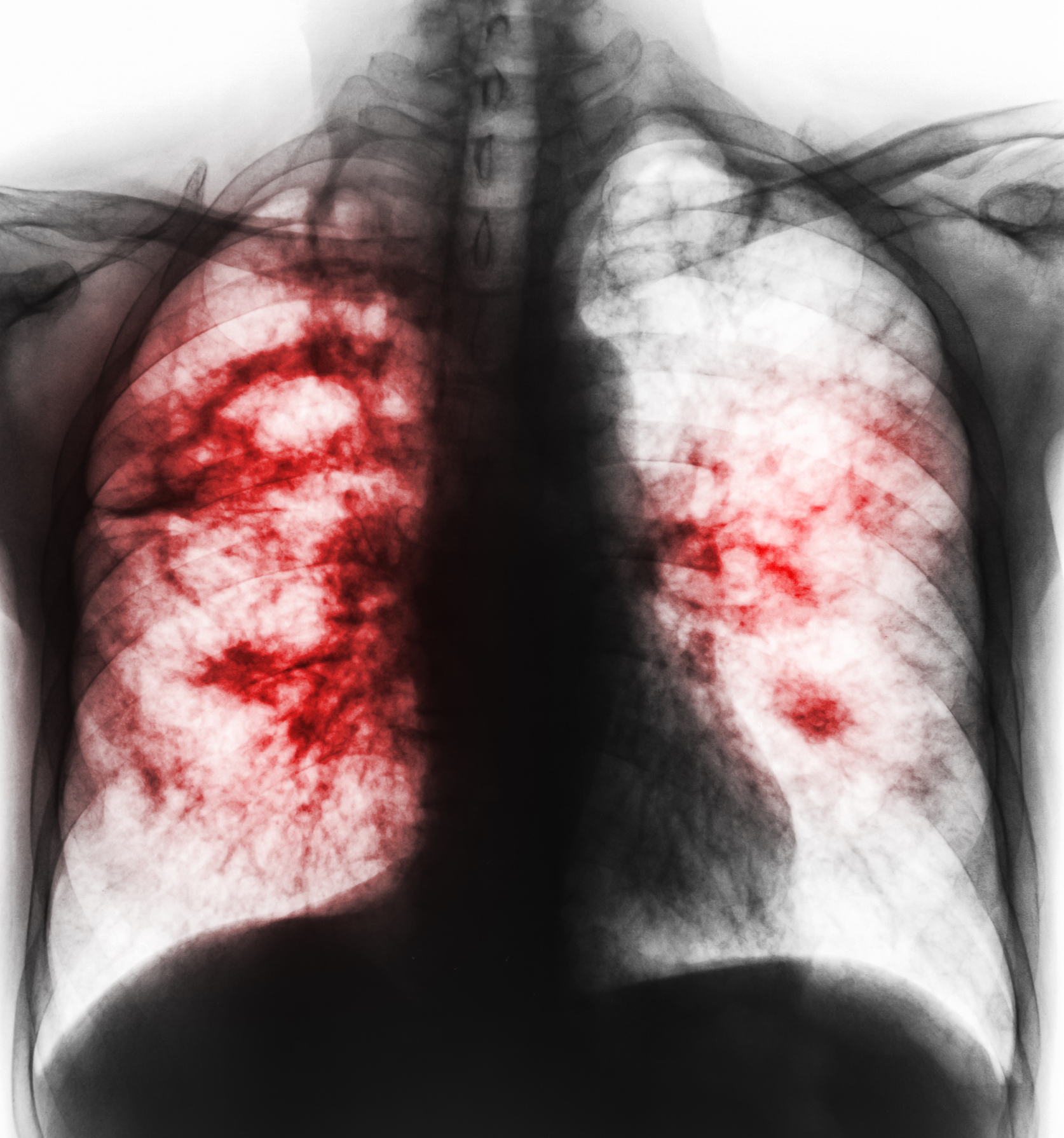
Experts Dr Michel Gasana & Dr Frank Lule from World Health Organization – Regional Office for Africa, provide an update on the global picture of Tuberculosis
Dr Michel Gasana, TB Medical Officer, World Health Organization (WHO) – Regional Office for Africa, spoke with Open Access Government to provide an update on the global picture of Tuberculosis (TB).
While TB mainly affects adults in their most productive years, we also find out how it impacts children. We learn why TB is particularly difficult to diagnose in children and about the Xpert MTB/RIF assay, generally available to assist with the diagnosis of paediatric TB.
Further into this in-depth interview, Dr Gasana walks us through how TB is treated and how WHO Africa responds to this bacterial infection. Finally, we discover how COVID-19 has affected the TB response in the continent.
What are your concerns about the global picture of TB?
An estimated 10 million people fell ill with TB worldwide in 2020, among which, 5.6 million were men and 3.4 million women, with 1.1 million children. 4.1 million were undiagnosed or not reported although the disease is preventable and curable to ensure global response to the fight against the TB epidemic and outlined concrete actions for increased investments and innovation. TB deaths were estimated to be 1.5 million in 2020.
2020 WHO Global TB Report showed improvement in indicators for TB in the African Region. There was good progress towards the End TB milestones for a reduction in TB incidence. In 2020, there was a 19% reduction in TB incidence. However, despite the progress in reducing TB incidence and implementing internationally recommended control strategies, TB remains a communicable disease of major public health importance in the African region.
The WHO Africa Region accounts for 25% of the estimated global TB burden but over 36% of global TB deaths. There is still a significant gap between estimated incidence and notifications – 44% of incident TB cases were not diagnosed or reported in 2020 – representing 1.1 million of TB. The major challenges are related to inadequacies in the identification of people including children with TB, for all TB and drug-resistant TB, prevention of TB and financing of the TB response.
The region hosts 17 and 22 of the top 30 countries with the world’s highest TB and HIV/TB burdens respectively. Around 73.5% of People Living With HIV who fell ill with TB are in Africa. No country has yet demonstrated that it has met the target that no TB -affected households face catastrophic costs.
Despite the toll of the disease, TB is not yet at the forefront of health priorities in countries. Engagement required from other development sectors to complement efforts made by the health sector is inadequate. Yet, while COVID-19 has galvanized global cooperation to drive decentralized access to diagnostics, rapid testing and vaccine production, efforts to end TB are often overlooked and underfunded.
While TB mainly affects adults in their most productive years, how does it impact children?
According to the latest World Health Organization (WHO) Global Tuberculosis Report, an estimated 1.1 million children (aged 0–14 years old) developed TB disease in 2020, and 226,000 died due to TB.
The number of children and adolescents notified to the WHO is substantially lower than these estimates; in 2020, approximately 400,000 children aged 0–14 years were notified of TB.
Gaps between notifications to the WHO and burden estimates stem from shortcomings in detection, diagnosis and reporting in these age groups. Today, it is estimated that more than 60% of all children with TB worldwide are never even diagnosed and 96% of children who die from TB are never put on treatment, 80% of them are younger than five years old. Most children less than five years old affected by TB die when they are not diagnosed and treated. Children aged less than five years are also more likely to progress to TB disease after infection and have the highest rates of severe, disseminated forms of TB such as meningitis, compared with older age groups.
In addition, children are at a much higher risk of developing active TB, especially when their immune systems are compromised by malnutrition, HIV or other diseases, which exacerbate the severity of the disease.

Why is TB particularly difficult to diagnose in children?
TB in children is clinically and epidemiologically heterogeneous, making care and prevention difficult. In children, TB is often complicated to diagnose due to non-specific symptoms which overlap with those of other common childhood diseases and limited sensitivity and specificity of laboratory tests for latent TB infection and TB.
Health systems in high TB burden countries (TB HBCs) are often overburdened, with limited capacity to recognise presumptive TB and poor access to diagnostic tools.
Delayed or missed TB diagnosis in children leads to an increased risk of rapid disease progression and mortality, especially in younger children.
Tell us about the Xpert MTB/RIF assay – generally available to assist with the diagnosis of paediatric TB
The new WHO guidelines include recommendations intended to bridge the diagnostic gaps in children and adolescents by expanding the specimen types that can be tested for TB using rapid molecular diagnostics beyond sputum and nasopharyngeal aspirates, to include gastric aspirates and stool which are easier to collect and less invasive.
Small children are often not able to produce sufficient sputum to test. In children with signs and symptoms of pulmonary TB, Xpert Ultra should be used as the initial diagnostic test for TB and detection of rifampicin resistance on sputum, nasopharyngeal aspirate, gastric aspirate or stool, rather than smear microscopy/culture and DST.
There are, however, limitations with the GeneXpert test for the following reasons:
• First the Genexpert machine is not often available outside urban settings or where electricity is available and the sites where most children need to be diagnosed.
• In addition, the machine needs a continuous power supply and an air-conditioned room.
• The high price of the GeneXpert machine and tests are also a limiting factor in the ability of countries to scale up testing.
• Maintenance issue: machines are frequently breaking down.
We urgently need better laboratory tests made available to all children with TB that work regardless of where they may live.
How is TB treated?
TB disease is treated with a combination of several medications for six months. The 6-month regimen has become the standard of care all over the world, but efforts have been made to develop effective shorter regimens to treat Drug Susceptible TB. The new guidelines offer shorter, safer and more child-friendly regimens for TB prevention and treatment of drug-susceptible and drug-resistant TB.
Currently, treatment of drug-susceptible TB using 4-month regimens for treatment of children with non-severe TB is available.
It is important that people who have TB disease finish the medicine and take the drugs exactly as prescribed by their doctor. If they stop taking the drugs too soon, they can become sick again. If they do not take the drugs correctly, the bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat.
Children with HIV have an increased mortality risk, even when receiving TB treatment.
How is WHO Africa responding to TB?
The WHO plays a global leadership role in health and particularly in the TB agenda: Adequate political and financial support to end, including childhood TB, is critical to move faster toward the global targets.
Recently, the continent adopted and endorsed the Africa Continental TB Scorecard and the Africa Continental End TB Accountability Framework for Action to track member states progress towards SDG and End TB Strategy targets commitments. It is updated each year and shared with state Members.
WHO Africa supports member states to adapt and adopt the latest policies and guidelines on TB and ensure that they are implemented at all levels of care.
WHO is advocating for increased investment in TB research to spur technological advances and rapid adoption of innovations in diagnostics, treatment and vaccines.
WHO is advocating to address barriers to accessing health and other social services, social determinants of health and progress towards UHC particularly for marginalized, under-served and vulnerable populations.
The paediatric agenda must become much more visible. WHO is advocating for children to have access to quality healthcare, and to be rapidly diagnosed and treated using tools that have been optimized for children.
How has COVID-19 affected TB response in the continent?
The coronavirus pandemic (COVID-19) caused huge health, social and economic impacts in 2020 and 2021. The COVID-19 pandemic has reversed years of progress in ending TB, with TB deaths increasing in 2020 for the first time due to disruption of access to TB services. The COVID-19 pandemic has affected the provision and access to essential TB services, including diagnostics and treatment. There has also been a reduction in the number of people that visited the health facilities for diagnosis and treatment due to lockdowns. In addition, some of the equipment used to diagnose TB was re-purposed to help with the response to the pandemic. Health workers were reassigned to support the response to the COVID-19 pandemic.
Mitigation measures: countries have put in place innovative means to address the problem of TB in the context of COVID by:
• Providing one month of TB drugs to patients and using video messaging to continue directly observed treatment as recommended by WHO and maintaining continuity of essential health services including TB.
• Using of artificial intelligence in chest x-ray devices to improve detection of TB cases.
• Using of shared laboratory platforms and equipment to improve COVID-19 and TB and HIV testing.








