Infections are the second leading cause of death in cancer patients, after the cancer itself; Zisis Kozlakidis and Shalini Jayasekar Zurn discuss the challenges surrounding the interplay between cancer and antimicrobial resistance (AMR)
Antimicrobial resistance (AMR) and cancer are two of the most pressing health challenges worldwide, and they intersect in complex and concerning ways. AMR refers to the ability of microorganisms, such as bacteria, viruses, and fungi, to survive exposure to antimicrobial medicines (e.g., antibiotics and antifungals for bacterial and fungal infections, respectively) that would normally kill them or inhibit their growth. As a result of this drug resistance, medicines become ineffective, and the infections (by viruses, bacteria, or fungi) become very difficult, if not impossible, to treat. Cancer, on the other hand, is characterised by the uncontrolled growth of abnormal cells in the body. Together, these two issues pose unique challenges in healthcare due to the role of antimicrobials in cancer treatment and the potential for antimicrobial-resistant infections to exacerbate cancer patients’ vulnerability.
How antimicrobial resistance impacts cancer care
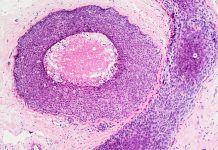
For cancer patients, AMR is particularly problematic because they are often more susceptible to infections due to their compromised immune systems. Chemotherapy, one of the most common cancer treatments, not only targets cancer cells but can also affect the body’s healthy cells, particularly in the bone marrow (which has an impact on the production of white blood cells/immune cells).
There are a number of improvements that have been made in the treatment type and method of administration for chemotherapies to minimise such effects on healthy cells, but in many cases, this side effect remains as yet unavoidable. As a result, this suppression of immune cells leaves cancer patients with a weakened immune defence, making them more prone to infections. If such patients are infected by antimicrobial-resistant pathogens (microorganisms that can cause diseases), then these infections will become very hard to treat. The World Health Organization estimates that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths. (1)
In the case of cancer patients undergoing intensive treatments, antibiotics are frequently administered prophylactically, i.e., to prevent and treat infections as part of the therapy.
However, the widespread use of antibiotics in these settings also increases the selection pressure on bacteria, contributing in this way to the emergence of resistant strains. This becomes a vicious cycle, as resistant strains may circulate and further strengthen within hospitals or oncology centres where immune-compromised cancer patients are treated, leading to hospital-acquired infections that are increasingly difficult to control. For example, Clostridioides difficile, a bacterium commonly associated with antibiotic use, is a significant threat to cancer patients because it can cause severe gastrointestinal illness, especially in those whose immune systems are compromised. This places cancer patients at a higher risk of morbidity and mortality from infections that would otherwise be manageable with available antibiotics – and, importantly, even if the original cancer treatment is successful. Infections are the second leading cause of death in cancer patients, after the cancer itself. (2)
This interplay between cancer and AMR is further complicated by certain antimicrobials’ potential to affect cancer treatment effectiveness. Some studies suggest that broad-spectrum antibiotics may impact the gut microbiota, which plays a significant role in regulating the immune system. A healthy gut microbiome is known to support immune responses against cancer, potentially influencing the success of therapies such as immunotherapy. Disrupting this balance through antibiotics may thus impair the body’s natural and therapeutic defence against cancer. Additionally, certain bacteria or fungi can also alter the local micro-environment of tumours, such that these tumours appear resistant to ongoing treatment. (3) This is a system that is very dynamic and driven by biological responses – yet only now started to be elucidated with the advent of high-throughput technologies such as whole genome bacterial sequencing.
Addressing AMR in cancer care
Addressing AMR in cancer care requires understanding a complex and dynamic biological system and, as a result, requires a multifaceted approach. First, there is a need for more balanced use of antibiotics, antifungals, and other antimicrobial medicines in cancer patients, balancing infection management to the individual in the short-term with the risk of resistance development that can affect others in the longer term.
Infection prevention and control measures in hospitals and cancer centres are also critical, particularly in establishing targeted surveillance programs and reducing the spread of resistant pathogens in these settings. Therefore, optimal use of existing therapies is critical via good stewardship practise. Furthermore, investing in the research and development of new antimicrobials and diagnostics, as well as alternative therapies (e.g., phage therapy), is essential to providing effective infection control and management for cancer patients. However, the latter is of particular concern as the world faces both an antibiotics pipeline and access crisis. In other words, there is an inadequate research and development pipeline in the face of rising levels of resistance and an urgent need for additional measures to ensure equitable access to new and existing vaccines, diagnostics, and antimicrobial medicines. (4)
Finally, it should be noted that while AMR exists in all settings (from low- to high-income), the impact is greatest in cancer patients in resource-restricted settings, as in the latter case, access to appropriate treatments may be limited. (5) Given the pressing challenges to cancer management posed by AMR, the Union for International Cancer Control, the oldest and largest cancer organisation globally, is committed to supporting the cancer community in efforts to address AMR. And set up an expert Task Force in 2020 to provide guidance in addressing AMR for better cancer care. (6)
AMR is a growing concern
AMR represents a significant and increasing complication in cancer treatment, threatening the safety and outcomes of patients who already face a daunting health battle. As the prevalence of AMR grows, it poses an increasing threat to the viability of cancer therapies. Addressing this issue requires coordinated efforts across healthcare systems, emphasising the need for responsible antimicrobial use, robust infection prevention and control practices, and innovation in treatment options to safeguard the lives of people living with cancer.
References
- Antimicrobial Resistance Collaborators. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet; 399(10325): P629-655. DOI: https://doi.org/10.1016/S0140-6736(21)02724-0
- Nanayakkara AK, et al. (2021) Antibiotic resistance in the patient with cancer: Escalating challenges and paths forward. CA Cancer J Clin. 71(6):488-504. doi: 10.3322/caac.21697
- Liu, NN, et al. (2022). Multi-kingdom microbiota analyses identify bacterial–fungal interactions and biomarkers of colorectal cancer across cohorts. Nature Microbiology, 7(2), 238-250.
- World Health Organization. (2022). Antimicrobial resistance – Key facts. Available online at: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- Union for International Cancer Control (UICC). (2022). Lack of access to antibiotics and antifungals compromises cancer care. Available online at: https://www.uicc.org/blog/lack-access-antibiotics-and-antifungals-compromise-cancer-care
- UICC (2024). Raising awareness about antimicrobial resistance. Available online at: Raising awareness about antimicrobial resistance | UICC