Katrina Delargy, Managing Director of TIYGA Health, tells us what we need to know about real-time symptom tracking for long COVID
“Speed trumps perfection. Perfection is the enemy of good when it comes to emergency responses” – the words of Dr Michael J. Ryan, WHO Executive Director, resonated around the world in March 2020. (1) He was referring to the spread of coronavirus, but this could apply to long COVID. WHO’s Director-General, Dr Tedros Adhanom Ghebreyesus, warned, “Long Covid has an impact on the individual, on society and on the economy,” highlighting the importance of the “three Rs” – recognition, research, and rehabilitation. (2)
Evidence suggests a “hidden iceberg” of undiagnosed COVID-19 people who are now suffering from long COVID. If 10-20% of all COVID-19 infections lead to long COVID, we could have 10-20 million long-term cases to manage. Finding a good approach to long COVID needs to be informed by real-time symptom data.
Year of the timeline
In 2020-21, daily freedoms have been dictated by the trends in COVID statistics. The numbers were often shocking and disturbing, but the really crucial issue was (and still is) the direction the numbers were going and the speed of change. Timelines became important.
Symptom reporting in real-time
2020-21 saw many forms of routine healthcare interaction being abandoned or become virtual and, in the minds of the public, there was increased vigilance for personal risk exposure. Never before have so many people been so vigilant for the appearance of new symptoms that might normally be dismissed. The list of symptoms that were associated with COVID-19 grew, helped by the daily reporting by over 4 million citizens who continue to use the King’s College Zoe COVID Study app for research. By making it easy, convenient and relevant researchers could obtain real-time data on symptom prevalence – and how long the symptoms lasted. This self-report data contributed to the overall national picture of the spread of infection.
Long COVID, post-COVID syndrome or post-viral fatigue?
Symptom reporting and analysis became central to the debates. For a long time, a key question was about how many asymptomatic carriers there were in the community or moving around. Increasingly the question of how long the symptoms of COVID-19 last. ‘Long COVID’ is commonly used to describe signs and symptoms that continue or develop after acute COVID-19.
The symptoms of long COVID (Post-Acute Sequelae of COVID-19 or PASC) are multisystemic/ multiorgan and now known to involve cell damage. NICE distinguishes between the acute phase (up to four weeks), the ongoing symptomatic phase (four to 12 weeks) and post-COVID-19 syndrome where signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis. Long COVID is not in the textbooks yet, the gold-standard clinical trials may have started and answers will hopefully evolve with trial results.
TIYGA: Voice of the patient
Much of the research on long COVID is now patient-led or patient-driven, it has to happen in real-time and relies on capturing data on what symptoms a person has, how those symptoms vary in intensity day by day and how long they last. National support groups are being formed to investigate clinically unknown parameters. TIYGA’s platform can accommodate both the wide range of symptoms and the requirement for ease of use by people suffering from fatigue and brain fog.
Long COVID relies on self-report of symptom data, TIYGA Health is engaging with local support groups to capture data. Analysis of such data can contribute to the determination of optimal pathways to the right specialists and investigations.
Early intervention
There are lessons to be learned from chronic pain and other complex conditions where the time delays between the patient seeing the GP, the GP making a referral and the pain management specialist giving a diagnosis can be several years – during which time the problem has become more difficult to solve. Part of this delay may be due to inconsistent history from the patient, vague signs or symptoms or scepticism from the healthcare provider. Precision medicine should be preventative, predictive, personalised and participatory. Long COVID affects people differently. Maybe we need a precision medicine approach, accelerating healthcare 4.0.
Right person, right treatment, right time, right place
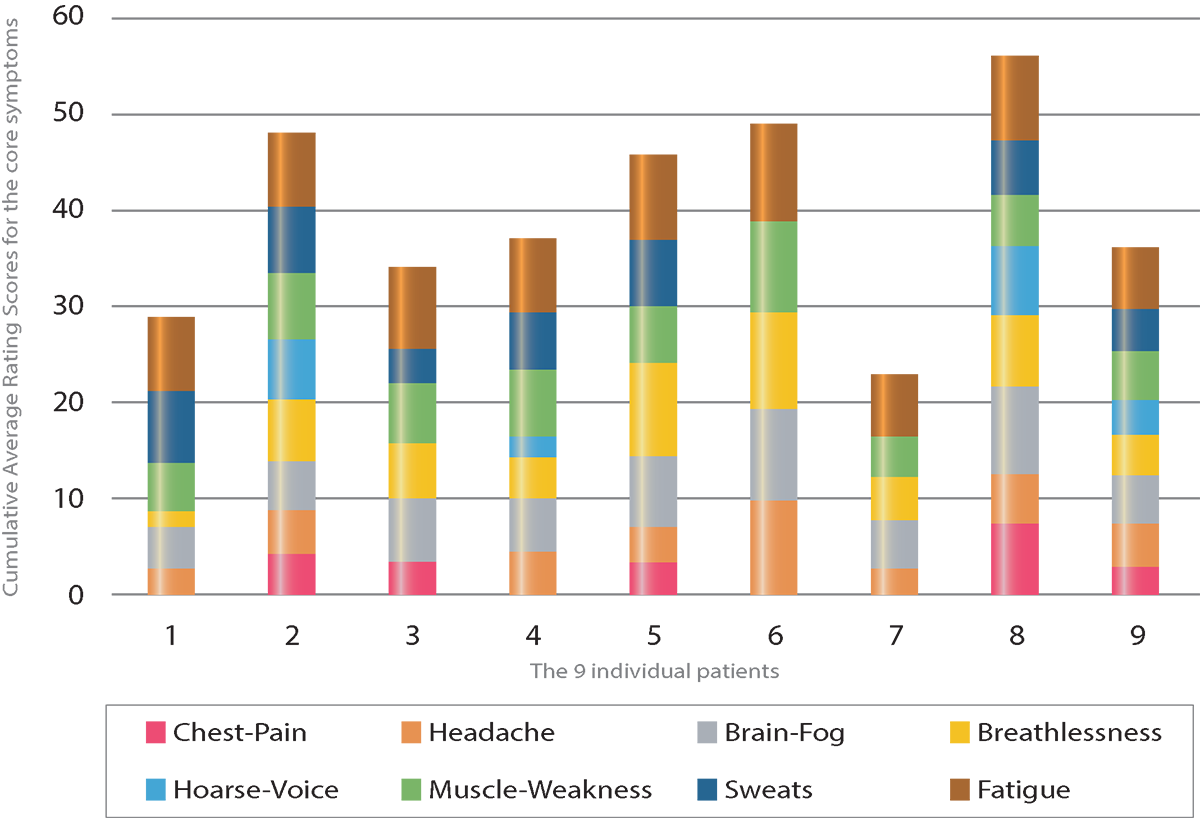
Certain therapies can be highly beneficial for some patients but can risk harm for patients with post-viral syndromes. Real-time symptom data can help us to understand which patients need to be fast-tracked to specialist teams. Activated digitally savvy patients are ready to embrace such approaches, as seen in Figure 1.
We need a dynamic and responsive approach that allows prediction of exacerbation which can support anticipatory personalised care. New hybrid models of care need to combine remote and place-based care and prioritise those at greatest risk. We cannot wait for a perfect model to be validated by researchers before adopting it in practice. Real-time symptom and activity tracking with smart analytics are vital to address the long COVID challenge.
References
1 https://twitter.com/ungeneva/status/1238740397901447168?lang=en
3 https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/long-coronavirus-symptoms-3-possible-signs-of-long-covid-as-per-cdc-doctor/photostory/82326989.cms
Please note: This is a commercial profile
© 2019. This work is licensed under CC-BY-NC-ND.











