Dr Nazneen Rahman, Founder and CEO of YewMaker and Sustainable Medicines Partnership (SMP) Director describes how integrating clinical, cost, and carbon effectiveness is key to delivering sustainable healthcare with the Triple-C framework
In 1994, John Elkington introduced the concept of the triple-bottom-line, which encouraged businesses to measure their success not only in terms of profit but also by considering their social and environmental impact. Over time, the concept has become increasingly important in corporate responsibility and is often distilled to three P’s – people, planet, and profit.
Interest in the triple-bottom-line within healthcare has increased with the recognition of the significant contribution of the health sector to greenhouse gas emissions. For example, the NHS is responsible for an estimated 4-5% of England’s carbon footprint and has committed to becoming net zero by 2045. However, despite the urgency, the practical implementation of the triple-bottom-line framework in healthcare has been limited.
At YewMaker the triple-bottom-line concept is central to our ambition to build science-based solutions to make healthcare more sustainable. However, we believe adaptation of the framework is needed to encompass the unique contexts of healthcare. The classic framework often places profit at the forefront with health under the social pillar, whereas healthcare organisations must prioritise patient impact, with economic and environmental impacts assessed in relation to their influence on clinical outcomes. Additionally, application in healthcare must be grounded in the methods used to measure and evaluate healthcare interventions.
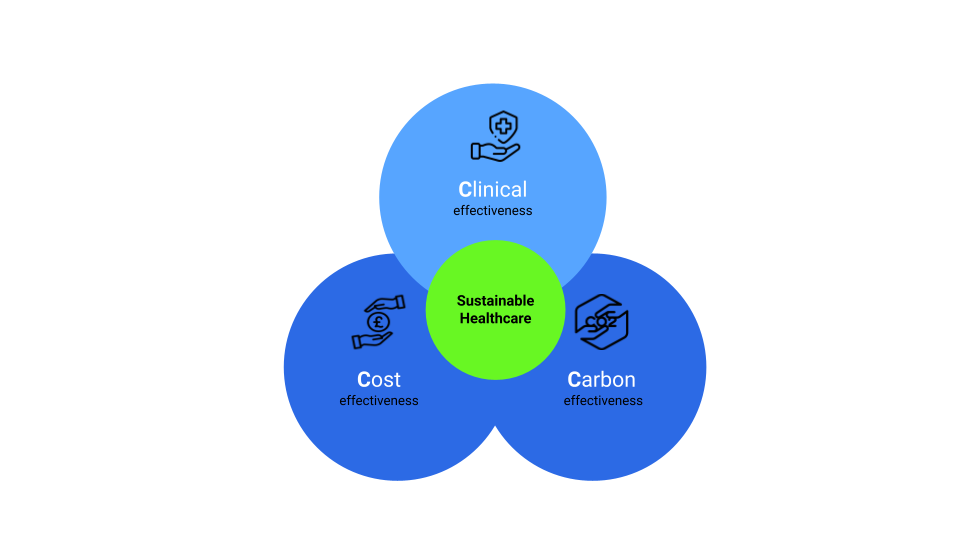
Introducing the Triple-C framework
To maximise usefulness, we suggest the application of the triple-bottom-line in healthcare could be distilled to the Triple-C framework – clinical effectiveness, cost-effectiveness, and carbon effectiveness.
- Clinical effectiveness is a measure of how well a treatment or intervention works in improving health outcomes, such as reducing mortality or symptom severity or enhancing the quality of life. A range of methods are used to evaluate the clinical effectiveness, with randomised controlled trials considered the gold standard. Clinical effectiveness should always be the primary measure.
- Cost-effectiveness is a measure of the value for money of healthcare treatments and interventions. In Cost-effectiveness analysis the costs of an intervention are compared against the benefits using outcome measures such as life years gained, quality-adjusted life years, or disease-specific outcomes.
- Carbon effectiveness refers to the extent to which a product, service or process reduces carbon emissions and mitigates climate change. It is a measure of the environmental impact of a given activity or operation. Carbon accounting is often used to evaluate carbon effectiveness, with life cycle assessment considered the most comprehensive approach.
The primary measure in the Triple-C framework should always be clinical effectiveness. The relative merits of cost and carbon effectiveness can be flexibly evaluated and weighted, as required. Triple-win interventions are those in which clinical effectiveness is also cost and carbon effective.
Triple-C framework in practice: MCF Classifier
We used the Triple-C framework in the design of MCF Classifier, a SBRI Healthcare supported software solution YewMaker is building to estimate the carbon footprint of medicines. Within MCF Classifier we stratify medicine carbon footprints per tablet into a categorical scale presented in a user-friendly carbon effectiveness RAG rating. Alongside, we present clinical and cost recommendations from the local Formulary so decision-makers have the necessary information to make a Triple-C framework evaluation of medicines.
Triple-C framework in practice – reducing overprescribing
Reducing overprescribing has been identified as an NHS priority. It is estimated 10% of primary care prescriptions are not needed and unnecessary medicines contribute to 6.5% of hospital admissions caused by adverse drug reactions. Reducing overprescribing is an excellent triple-win opportunity that will reduce clinical harm, costs, and emissions. Using MCF Classifier, we can estimate the carbon effectiveness of tackling overprescription. For example, ~20% of primary care antibiotic prescriptions are considered to be unnecessary. Using MCF Classifier we estimate a 20% reduction in primary care prescriptions of penicillins in England in 2021 would have saved £4 million and 31 ktCO2e in emissions which is equivalent to flying 22 times around the world.
Practical frameworks are needed for action
We urgently need to deliver sustainable healthcare, healthcare that maximises the health and well-being of our populations whilst minimising unnecessary costs and damage to our planet. Practical metrics and frameworks that facilitate understanding and action are essential. We hope the Triple-C framework will be a useful starting point.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.











