Romola Davenport and Richard Smith from the University of Cambridge explore epidemiological interactions between rural and urban populations and the consequences of urbanisation
Today, urban populations almost always have higher life expectancies than their rural counterparts, because cities provide better access to health facilities, clean water and sanitation and because urban dwellers tend to be richer. However, this pattern is a very modern one. Before the early twentieth-century rural populations were almost uniformly healthier than urban ones. Indeed, in the centuries before c.1770, European cities were characterised by death rates so high that their populations would have imploded without a reliable stream of rural migrants. Some scholars have argued that this ‘urban graveyard’ effect imposed an upper limit on the levels of urbanisation and therefore, economic growth that those pre-modern societies could sustain because cities imposed such a drain on the populations of their rural hinterlands.
For rural migrants to towns, the health costs of immigration were high. Before the twentieth century, towns were characterised by much higher levels of infectious diseases, especially gastrointestinal diseases, as a consequence of inadequate sanitation and so-called ‘crowd’ diseases that relied on high population densities for transmission
For those born in towns, these diseases took their greatest toll in childhood, when diarrhoeal diseases were most lethal, and when many diseases were encountered for the first time. For urban-born adults, the disadvantages were not so great, because those who survived to adulthood had already encountered and developed some immunity to many of the most dangerous urban diseases. Migrants, however, were in an immunological sense akin in some ways to young children. Many rural migrants came from areas where diseases, such as measles and smallpox were rare, and they often arrived in cities with no immunity to these diseases.
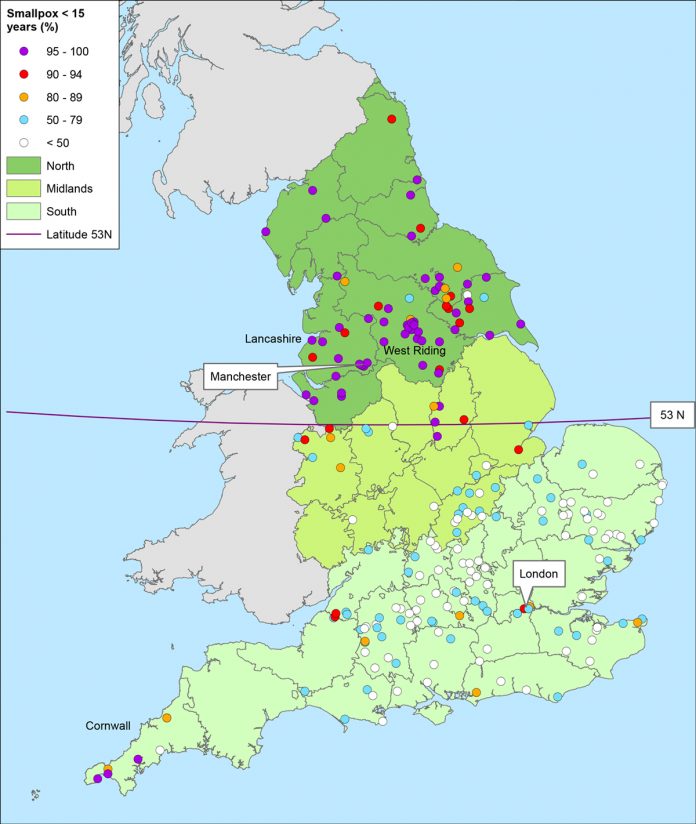
The consequences of these differences in disease exposure in rural and urban areas are strikingly illustrated in the case of smallpox. Before the introduction of vaccination c.1800, smallpox was the single most lethal disease of eighteenth-century Britain, accounting for up to 10% of all deaths in southern England and up to 20% in the north.
In eighteenth-century London, smallpox was pre-eminently a childhood disease, with deaths concentrated amongst children under seven. However, there was a second bulge of smallpox deaths amongst young adults, primarily when young migrants arrived for the first time in London. Although probably taller on average than their urban-born peers and healthier than the rural populations they left behind, these young economic migrants contributed to high urban death tolls.
Before vaccination, the dangers of smallpox to rural migrants to towns depended on the extent to which smallpox patterns differed between towns and their migrant hinterlands. In southern England, smallpox was a rare epidemic disease outside the largest cities and many rural dwellers survived to adulthood without infection.
However, in northern Britain smallpox circulated as a childhood disease throughout rural as well as urban areas. As a consequence, very few migrants died of smallpox in northern towns because they were already immune. This north-south difference in patterns of circulation of smallpox in rural populations appears to have arisen from differences in local responses to smallpox.
In the south, smallpox victims were isolated, and markets closed to prevent outbreaks. In addition, once inoculation (a forerunner of vaccination, involving immunisation with a low dose of smallpox) became popular then many southern parishes performed occasional mass immunisations of the entire vulnerable population to prevent outbreaks. Northern communities did not adopt these tactics, possibly because they lacked the means to provide publicly-funded isolation facilities and free mass inoculations. The circulation of smallpox as a childhood disease throughout northern Britain increased smallpox mortality in rural areas, but also reduced the mortality gradient between town and country, lessening the risks of rural-urban migration in the north compared with southern Britain.
After 1800, the enormous decline in smallpox infection with vaccination made cities substantially safer for young children and for especially southern migrants. Vaccination made a major contribution to reducing urban mortality rates and in reducing the human and demographic costs of the unprecedented urbanisation that accompanied industrialisation. As a consequence of vaccination, changes in urban breastfeeding habits and other as yet unidentified factors, mortality in British cities had fallen by the early nineteenth century to the point where urban populations could reproduce themselves and cities acted to brake, but not to reverse population growth. Further improvements in water supplies, housing, income and sanitation were required to reverse the urban-rural gradient to the point where urban life expectancies exceeded rural (a point reached by the 1930s).
However, the example of smallpox illustrates the complex interplay of pathogen life histories, local policies, migration patterns and immunisation and other disease control strategies that continue to influence epidemiological interactions between rural and urban settlements. These interactions are historically contingent, a point that has given fresh force by recent reversals of urban-rural life expectancies in some affluent nations as a consequence of urban deprivation and changes in the main causes of death.
Richard Smith
Emeritus Professor of Historical
Demography and Geography
University of Cambridge
Tel: +44 (0)1223 333 182
https://www.campop.geog.cam.ac.uk/research/project/migrationmortalitymedicalisation/