Research from the University of Liverpool indicates that administering antibiotics alongside antimicrobials could lower death rates from malaria and meningitis
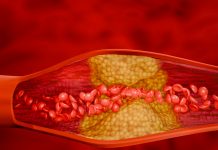
Fever and coma are commonly seen in African children, caused by malaria of the brain, followed by bacterial meningitis. However, these diseases have very similar symptoms, and the limited diagnostic testing makes them challenging to diagnose and treat.
The research, published in The Lancet Global Health, is the most extensive analysis of febrile non-traumatic coma in children on the African continent to date.
One in four African children with malaria and coma has an additional infection
The researchers analysed two parallel studies: The aetiology, mortality and disability of non-traumatic coma in African children: A systematic review and Aetiology, neuroradiological features, long-term neurosequelae and risk factors for mortality of febrile coma in Malawian children: A prospective cohort study.
The first study reviewed all previous studies for non-traumatic coma in African children and found that the death rate due to malaria infection has remained unchanged for nearly fifty years, with almost one in every five children dying. This is despite years of research and interventions such as bed nets and improved treatments.
The second study found that cerebral malaria is the leading cause of febrile coma and that co-infections complicated over a quarter of cases. These infections were mainly bacterial and detected through molecular tools. The research showed that children with malaria and bacterial meningitis co-infection were more likely to die, compared to those with malaria alone, and the risk of death was even greater if co-infected children did not receive antibiotics.
These findings highlighted the urgent need to re-consider frontline management for children who present with fever and coma and indicate the critical need for immediate antibiotics (alongside antimalarials), irrespective of malaria diagnosis.
Dr Stephen Ray, Principal Investigator at the Oxford Vaccine Group led the study alongside Dr Charlotte Fuller, from the Brain Infection and Inflammation Group at the University of Liverpool.
Dr Ray said: “Too often malaria parasites found in the blood of a sick African child stop medical staff from looking for and treating additional bacterial infections. A positive malaria test commonly leads to only treating the child with antimalarials, and therefore it becomes a risk factor for children to die from untreated bacterial infections. Our study found there were frequent bacterial infections, often alongside malaria, and these results emphasise the need for immediate antibiotics to be given to all children presenting with fever and coma, even if they have a positive malaria test. Our hope is that these findings cause a change in practice and save lives”.
The findings will support the World Health Organization
The researchers performed an MRI at admission and identified that 90% of children had a brain injury and 50% had brain swelling at hospitalisation. They also found most children with meningitis had severe complications, such as intracranial pus, that could have been treated earlier with neurosurgery.
Additionally, the team performed face-to-face neurological follow-up assessments with survivors and identified a disability in half of these children. The findings support an update of national and WHO guidelines on severe malaria and coma, and changes to clinical practice.
University of Liverpool’s Dr Charlotte Fuller said: “Our cohort study highlights the value of molecular and radiological diagnostics in managing life-threatening brain infections. The frequent complications found on admission brain scans illustrate that earlier escalation to specialist care, with neurosurgical capacity, maybe most critical. Further work is needed to facilitate widespread deployment of affordable molecular and radiological diagnostics across the African continent”.