Sarah Woolnough, CEO of Asthma UK and the British Lung Foundation, reflects on landmark research undertaken by the charity ahead of World COPD Day, including the largest ever survey of people with COPD in the UK
COPD is the poor relation of chronic diseases, shown by the huge drop in people being diagnosed last year compared to other chronic conditions.
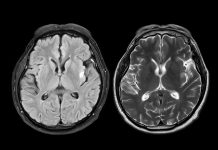
Millions of people in the UK live with COPD, or chronic obstructive pulmonary disease, an umbrella term for a group of lung conditions that make it harder to move air in and out of the lungs. It’s a cruel condition, which can force people to quit their jobs and make day-to-day activities like housework impossible. There is no cure for COPD, but early diagnosis and proper care can help people live longer and more comfortable lives. Heartbreakingly, however, our new research exposes totally unacceptable levels of delay in diagnosis and care that fails on the fundamentals.
Millions may be missing out on diagnosis
If around half of cancer cases went undiagnosed, it would be a national scandal. And yet, this is exactly the situation with COPD. About 1.3 million people in the UK have a diagnosis of COPD, and it’s estimated that at least a similar number of people have the condition but don’t know it, because they haven’t been diagnosed. This means over a million people could be living with this fatal disease without any treatment or care.
This alarmingly low rate of diagnosis has been made even worse by the COVID-19 pandemic. GPs were advised by NHS England in March 2020 to stop using diagnostic breathing tests known as spirometry tests. This, coupled with difficulty in people getting appointments, led to a 51% reduction in COPD diagnoses in England alone in 2020 – that’s around 46,000 people missing out on a diagnosis. This is a much larger percentage drop than seen for other conditions such as heart disease, heart failure, stroke and diabetes. GPs being asked to stop spirometry was reasonable at the time, given the emerging COVID-19 virus. However, despite guidance now advising it is safe to resume spirometry, many GPs have not yet restarted services, making it likely that a further 46,000 people in England may have gone undiagnosed in 2021.
However, even before the pandemic, the situation was dire. Many patients report being sent away from their GP surgeries or being initially misdiagnosed, often with a cough or chest infection. Public awareness is low and there are long-standing misconceptions about COPD, most commonly that it only affects smokers and older people. In fact, one in ten people who have COPD have never smoked, and our research shows more than one in five people were under 45 when they first started noticing their COPD symptoms.
Failing on fundamental care
Sadly, the problems don’t end after diagnosis. The standard of care many people receive for their COPD is low, with almost one million people missing out on the very basics.
NICE has defined its five fundamentals of COPD care: a written self-management plan, access to pulmonary rehabilitation, assistance to stop smoking, identification and management of coexisting medical conditions, and flu and pneumonia vaccination. Every person with COPD should expect these as standard, but our survey shockingly finds that 75% of people are missing out on at least one of these five.
Proper basic care helps people with COPD manage their condition and can help stop exacerbations that require more extreme interventions. It’s vital, then, that people with COPD access basic care right from the start. However, our research finds that patients who have only recently been diagnosed with COPD are the most likely to receive substandard care. This may be because people who’ve been living with the condition for longer are more used to navigating the healthcare system, and also perhaps that patients are only likely to start getting the care they need when their COPD is more advanced and their health has already deteriorated.
With so many missing out on basic care, far more people end up in hospital. COPD is the second largest cause of emergency hospital admissions, higher than the likes of diabetes. Not only do these hospital admissions cause patients and their families untold suffering, they also put a significant burden on our health service – it is estimated that COPD costs the NHS a staggering £1.9 billion a year.
We cannot carry on like this
People living with COPD have been forgotten and left behind by health systems for too long. We cannot sit back and watch as thousands of more people miss out on the diagnosis and care they so desperately need to live a happier, longer life.
While respiratory conditions are supposedly a clinical priority, as we approach the end of 2021 there is no plan to address the huge backlog in respiratory care, and diagnostic services are not yet back up and running. As a first step, we need rapid investment to help respiratory services get back on their feet, especially in primary care, and we need to see ambitious targets for improving COPD diagnosis and care. In England and Scotland, this means getting back on track with the respiratory ambitions set out in the NHS Long Term Plan and the Respiratory Care Action Plan respectively, and national health services must work with clinicians and patients to develop a new Respiratory Health Delivery Plan in Wales and a Lung Health Strategy in Northern Ireland as an urgent priority.